Tarek Sawas, Advanced Endoscopist at UT Southwestern, made the following post on X:
“Managing Barrett’s Esophagus (BE) is critical for preventing esophageal adenocarcinoma (EAC). Let’s dive into the latest American Gastroenterological Association (AGA) guideline on Endoscopic Eradication Therapy (EET) for BE and Related Neoplasia from AGA.
- The incidence of EAC has risen 5-fold since the 1970s.
- BE is the only known precursor of EAC.
- EET for dysplasia & early-stage cancer has revolutionized BE management, reducing esophagectomy morbidity/mortality and preventing EAC.
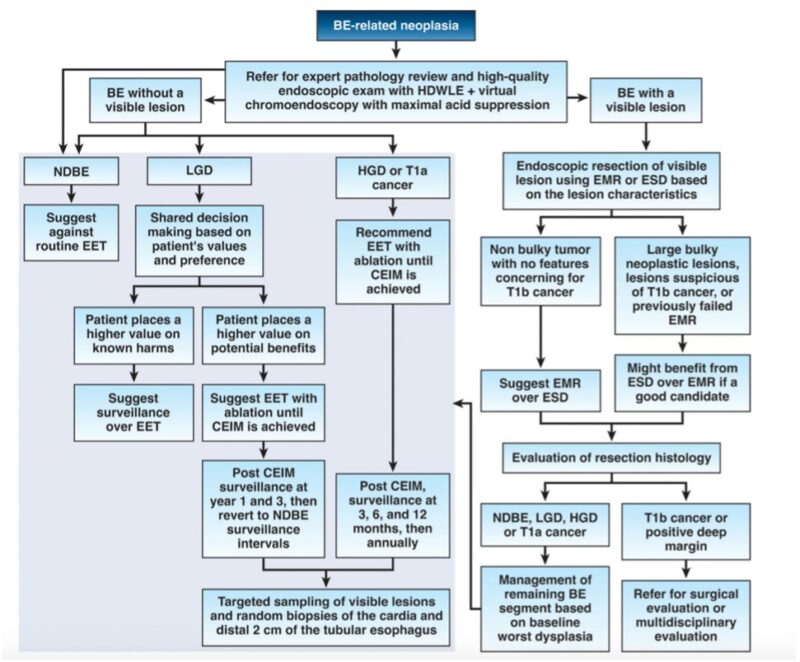
Who should undergo EET?
- BE with high-grade dysplasia (HGD), EET is recommended over surveillance.
- BE with low-grade dysplasia (LGD), EET is suggested over surveillance. Patients valuing the known risks over uncertain benefits might choose surveillance.
The primary goal of EET is complete eradication of intestinal metaplasia and neoplasia.
Routine use of EET is not recommended for NDBE patients
In EET, should we resect the entire BE segment or just visible lesions?
- Resection of visible lesions followed by ablation of the remaining segment is suggested.
When choosing between endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR) for visible lesions, either can be used based on lesion characteristics.
- Most neoplastic lesions can be managed with EMR.
- large, bulky lesions, those suspicious for deeper invasion (T1b) or failed EMR may benefit from ESD.
Before starting EET, discuss risks, benefits, reflux management, expected outcomes, and the need for continued surveillance with patients. Patient values and preferences are crucial.
Refer patients with dysplastic BE to high-volume endoscopists and pathologists with expertise in BE neoplasia and access to multidisciplinary care. Expertise matters!
Join us for Gastro Bites on Tuesday, June 11 at 12 p.m. ET where Drs. Sachin Wani, Joel Rubenstein, Swathi Eluri and I will discuss the key takeaways and best implementation considerations. Register.”
Read further.
Source: Tarek Sawas/X