Craniopharyngioma in Children: What patients and caregivers should know about
What is Craniopharyngioma?
Pediatric craniopharyngioma is a rare, benign brain tumor that arises near the pituitary gland and hypothalamus, crucial areas for hormonal regulation and neurological function. Despite being non-cancerous, these tumors can cause significant health issues due to their location, leading to symptoms such as visual disturbances, hormonal imbalances, and cognitive challenges. Typically diagnosed in children aged 5 to 14, craniopharyngiomas require careful management to mitigate their impact on the developing brain and overall health.
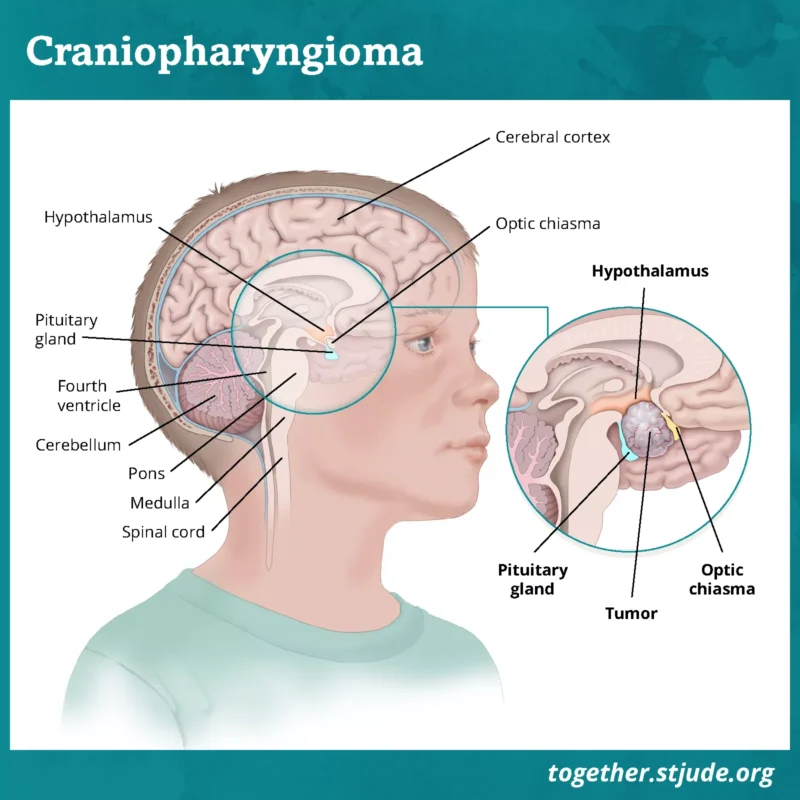
The image is taken from the website of St. Jude Children’s Research Hospital.
Prevalence and Epidemiology
Craniopharyngiomas account for approximately 1.2-4.6% of all intracranial tumors in children and are the most common pediatric suprasellar tumor. The incidence rate is about 0.5 to 2 cases per million persons per year. These tumors are typically diagnosed in children aged 5 to 14 years, with a slight male predominance.
Types
Craniopharyngiomas are histologically benign and can be classified into two main subtypes:
- Adamantinomatous craniopharyngioma (ACP)
- Papillary craniopharyngioma (PCP)
ACP is more common in children and is characterized by cystic formations and calcifications. PCP is more commonly seen in adults and lacks the cystic and calcified features of ACP.
Causes and Risk Factors
The exact cause of craniopharyngiomas is unknown. They are thought to arise from embryonic remnants of Rathke’s pouch, a structure involved in the development of the pituitary gland. There are no known genetic or environmental risk factors associated with these tumors.
Symptoms
Craniopharyngiomas produce symptoms by compressing adjacent neural structures, most importantly the optic pathways, hypothalamus, and pituitary gland. Symptoms can vary widely depending on the tumor’s size and location. Common symptoms include:
- Headache: Often due to increased intracranial pressure, headaches are present in 60-80% of children at diagnosis.
- Visual Impairment: Vision changes, including loss of visual acuity, visual field defects, and papilledema, occur in 20-60% of patients.
- Endocrine Dysfunction: Hormonal deficiencies are common, with growth hormone deficiency, hypothyroidism (when the thyroid gland doesn’t produce enough hormones), and diabetes insipidus (when the kidneys can’t conserve water, leading to excessive thirst and frequent urination) being the most frequent.
- Hydrocephalus: Tumor obstruction of cerebrospinal fluid pathways can lead to hydrocephalus, causing nausea, vomiting, and headache.
- Behavioral and Cognitive Changes: Cognitive deficits, emotional problems, and changes in behavior are prevalent among long-term survivors.
Diagnosis
Diagnosis of craniopharyngioma involves a combination of clinical evaluation, imaging studies, and laboratory tests.
Diagnostic tests include:
- Neurological Examination: To assess reflexes, muscle strength, coordination, and sensory function.
- Imaging Studies: MRI is the preferred imaging modality to visualize the tumor and its relationship to surrounding structures. CT scans may also be used to detect calcifications.
- Hormonal Tests: Blood tests to evaluate pituitary function, including levels of growth hormone, thyroid-stimulating hormone, adrenocorticotropic hormone, and others.
Treatment Options of Pediatric Craniopharyngioma
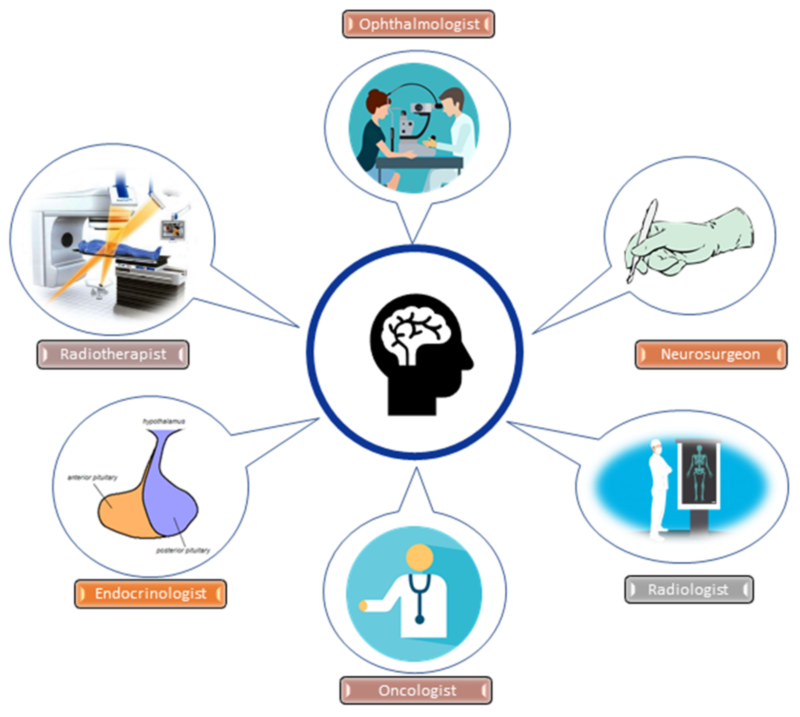
The treatment of craniopharyngiomas typically involves a multidisciplinary approach, combining surgical intervention, radiotherapy, and hormonal replacement therapy. The specific treatment plan is tailored to each individual patient, considering factors such as age, tumor characteristics, and potential risks and benefits.
Surgery
Surgery is the primary treatment for craniopharyngioma. The goal is to remove as much of the tumor as safely possible while minimizing damage to surrounding structures. Surgical options include:
- Gross Total Resection: Complete removal of the tumor, which is associated with better outcomes but carries a high risk of morbidity.
- Subtotal Resection: Partial removal of the tumor, often followed by adjuvant radiation therapy to control residual disease.
- Endoscopic Surgery: Minimally invasive approach for tumors with significant intrasellar components.
Radiation Therapy
Radiation therapy is used to treat residual tumor after surgery or as a primary treatment for inoperable tumors. Techniques include:
- Conventional Radiation Therapy: Typically given daily over six weeks.
- Stereotactic Radiosurgery: A precise form of radiation that targets the tumor while sparing surrounding tissue.
- Proton Beam Therapy: Preferred for its ability to minimize damage to adjacent brain structures.
Intracystic Therapy
For cystic craniopharyngiomas, intracystic therapies involve the instillation of agents such as radioactive phosphorus P-32, bleomycin, or interferon-alpha to reduce cyst size.
Hormone Replacement Therapy
Patients with pituitary dysfunction require lifelong hormone replacement therapy to manage deficiencies in growth hormone, thyroid hormone, cortisol, and sex hormones.
Emerging Therapies
- Targeted Molecular Therapies
- BRAF/MEK Inhibitors: Targeting the BRAF-V600E (lead to the production of an abnormal protein that drives cell growth and division) mutation found in some craniopharyngiomas, showing promising responses.
- Anti-IL-6: An IL-6 receptor antagonist, with reported effectiveness in slowing tumor progression.
- Immunotherapy
More information about completed and ongoing clinical trials for pediatric craniopharyngioma can be found here – clinicaltrials.gov.
Patient Survivorship
Long-term survivors of pediatric craniopharyngioma often face significant challenges due to the tumor and its treatment. Common issues include:
- Endocrine Dysfunction: Nearly all survivors experience some degree of pituitary insufficiency, requiring lifelong hormone replacement. Regular endocrinological assessments and appropriate hormone replacement therapy are essential. Growth hormone therapy, thyroid hormone replacement, and cortisol replacement are commonly required.
- Visual Impairment: Persistent vision problems are common, affecting up to 80% of survivors. Regular ophthalmological evaluations and interventions such as corrective lenses or surgery for severe cases. Early diagnosis and treatment of visual deficits can improve outcomes.
- Neurocognitive Deficits: Cognitive, psychosocial, and emotional problems are prevalent, impacting quality of life and academic performance. Multidisciplinary care involving neuropsychologists, educational specialists, and mental health professionals. Cognitive rehabilitation and individualized education plans can help address learning difficulties and behavioral problems.
- Hypothalamic Obesity: Damage to the hypothalamus can lead to severe obesity, which is difficult to manage and associated with increased morbidity. Intensive lifestyle interventions, including dietary modifications and physical activity as well as pharmacological treatment may be considered.
- Recurrence: Regular follow-up with MRI scans to monitor for tumor recurrence. Early intervention with surgery or radiation therapy can help manage recurrent disease.
Recommendations for Patients and Caregivers
- Seek Multidisciplinary Care: Ensure care is coordinated by a team of specialists, including neurosurgeons, endocrinologists, ophthalmologists, oncologists, and psychologists. A multidisciplinary approach is crucial for addressing the complex needs of these patients.
- Adhere to Regular Follow-Up: Maintain a strict follow-up schedule with regular imaging (MRI) and endocrinological assessments to monitor for tumor recurrence and manage long-term complications. Early detection and intervention for recurrence or complications can improve outcomes.
- Seek Educational and Psychosocial Support: Obtain educational support to address cognitive and behavioral issues that may arise. Engage with support groups and counseling services to help manage the emotional and social challenges faced by patients and families.
- Promote a Healthy Lifestyle: Encourage a balanced diet and regular physical activity to manage weight and overall health, as hypothalamic obesity is a common issue. Lifestyle interventions can help mitigate the long-term effects of hypothalamic dysfunction.
- Stay Informed and Advocate: Stay up-to-date with the latest research and treatment options for pediatric craniopharyngioma.
Advocate for the best possible care and support for your child, as treatment decisions can be complex and challenging. - Address Fatigue and Psychological Needs: Explore underlying causes of fatigue, such as sleep problems, hormone imbalances, or psychosocial factors. Seek psychological support to address emotional and mental health needs, as psychological well-being influences long-term health outcomes
- Prioritize Early Diagnosis: Be aware of the potential manifestations of hypothalamic dysfunction, as early diagnosis is crucial to prevent irreversible damage. Promptly report any concerning symptoms, such as vision changes, growth problems, or endocrine abnormalities, to healthcare providers.
Prognosis
The prognosis for pediatric craniopharyngioma is generally good, with an 80-90% chance of cure. However, the long-term prognosis is complicated by the high rate of recurrence and significant treatment-related morbidities, including endocrine dysfunction, visual impairment, and neurocognitive deficits
Factors Influencing Prognosis
Several factors influence the prognosis of pediatric craniopharyngioma, including:
- Age at Diagnosis: Younger age at diagnosis, especially under 5 years, is associated with a higher risk of recurrence and complications.
- Tumor Size and Location: Larger tumors and those involving the hypothalamus are more challenging to treat and are associated with worse outcomes.
- Extent of Surgical Resection: Complete resection without significant morbidity is ideal, but subtotal resection followed by radiation therapy is often necessary to preserve function.
- Histological Type: Adamantinomatous craniopharyngiomas have a higher recurrence rate compared to papillary types.
Conclusion
The journey of managing pediatric craniopharyngioma is undoubtedly challenging, but advancements in medical science and a multidisciplinary approach offer hope and improved outcomes for affected children. With the integration of precise surgical techniques, innovative radiotherapy options, and emerging targeted therapies, the prognosis for pediatric craniopharyngioma continues to improve. By staying informed, seeking comprehensive care, and leveraging the latest treatment modalities, patients and caregivers can navigate this complex condition with confidence and optimism. The collaborative efforts of healthcare professionals, researchers, and support networks are paving the way for a brighter future, ensuring that children with craniopharyngioma can lead fulfilling lives despite the challenges posed by this condition.
In this video, Declan shares his experience as a craniopharyngioma patient. The video is produced by Johns Hopkins Medicine.
Resources
- American Cancer Society – cancer.org
- National Cancer Institute – cancer.gov
- American Brain Foundation
- American Society of Clinical Oncology – asco.org
- Dana-Farber Cancer Institute – dana-farber.org
- Children’s Hospital of Philadelphia – chop.edu
- St. Jude Children’s Research Hospital
- Multidisciplinary Management of Craniopharyngiomas in Children: A Single Center Experience – Diagnostics
