HER2-low expression has recently been identified as a clinically relevant category in breast cancer. Defined as IHC 1+ or 2+ with negative FISH, it represents almost half of all breast cancers. Once considered part of the HER2-negative group, it has gained attention after the development of antibody–drug conjugates such as trastuzumab deruxtecan, which have demonstrated meaningful clinical activity.
Its role is particularly important in triple-negative breast cancer (TNBC), an aggressive subtype lacking hormone receptors and HER2 amplification. TNBC accounts for 15–20% of cases worldwide and is associated with poor prognosis and few targeted options. Clarifying whether tumors with low HER2 expression differ from those with no expression has become an important area of investigation.
To address this, a large multicenter study involving 40 Chinese hospitals examined clinical characteristics, genetic alterations, chemotherapy response, and survival outcomes in patients with HER2-low compared with HER2-zero TNBC. Complementary analyses using The Cancer Genome Atlas (TCGA) further explored genomic and transcriptomic profiles, offering insight into potential therapeutic opportunities.
Title: Clinicopathological and molecular significance of HER2-low expression in Asian women with triple-negative breast cancer
Authors: Cuiyan Yang, Haoyu Wang, Yiwei Tong, Zheng Wang, Xi Sun, Anqi Li, Yujie Lu, Mengyuan Han, Siji Zhu, Lei Dong, Kunwei Shen, and Xiaosong Chen
Published in Therapeutic Advances in Medical Oncology, August 2025
Background
Breast cancer remains the most common malignancy and a leading cause of cancer mortality among women worldwide. Triple-negative breast cancer (TNBC), characterized by lack of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2), accounts for 15%–20% of breast cancers and carries the poorest prognosis.
Traditionally, HER2 has been classified in a binary fashion as positive or negative. However, the concept of “HER2-low,” defined as IHC 1+ or IHC 2+ with negative FISH, has emerged and represents approximately 45%–55% of breast cancers. While anti-HER2 therapies have historically excluded these tumors, the recent success of antibody–drug conjugates (ADCs), such as trastuzumab deruxtecan, has highlighted HER2-low as a clinically meaningful category. Yet, the biological and clinical significance of HER2-low TNBC, particularly in Asian populations, remains unclear.
This multicenter study comprehensively examined clinicopathologic characteristics, homologous recombination repair (HRR) gene mutations, treatment response, and survival outcomes of HER2-low compared with HER2-zero TNBC in Asian women. Additional molecular analyses using The Cancer Genome Atlas (TCGA) dataset further explored the transcriptomic and genomic landscape.
Methods
The study retrospectively analyzed early-stage TNBC patients who underwent surgery between 2009 and 2021 across 40 Chinese medical centers contributing to the Shanghai Jiao Tong University Breast Cancer Database. Eligible patients had tumors ≥1 cm, complete clinicopathological and follow-up data, and, if treated with neoadjuvant chemotherapy (NAC), at least four cycles.
Targeted sequencing of 32 cancer-related genes, including 17 HRR-associated genes (e.g., BRCA1, BRCA2, PALB2, CHEK2), was performed in 360 patients. Pathological response and survival were assessed using standardized criteria. TCGA data (92 TNBC patients) were leveraged for transcriptomic and genomic analyses.
Study Design
The primary objective was to compare HER2-low (IHC 1+ or 2+ without amplification) versus HER2-zero (IHC 0) TNBC in terms of clinicopathologic features, HRR mutation spectrum, NAC response, and survival outcomes. Secondary analyses included molecular profiling of HER2-low TNBC through TCGA RNA-seq data, pathway enrichment analyses, and subgroup comparisons by gene mutations such as PIK3CA.
Results
Patient Cohort
A total of 3,376 Asian TNBC patients were included. Of these, 47.7% (n=1,611) were HER2-low and 52.3% (n=1,765) were HER2-zero. HER2-low TNBC was significantly associated with:
- Postmenopausal status (61.9% vs 49.4%, p<0.001)
- Family history of breast/ovarian cancer (5.5% vs 4.0%, p=0.04)
- Lymph node involvement (32.8% vs 28.6%, p=0.008)
- Invasive ductal carcinoma histology (69.3% vs 64.7%, p=0.004)
- Higher lymphovascular invasion (9.8% vs 7.7%, p=0.035)
- Lower Ki-67 proliferation rates (≤30%: 32.1% vs 27.4%, p=0.002)
Genomic Landscape
In the HRR-tested cohort (n=360), BRCA1 mutations were less frequent in HER2-low tumors (7.0% vs 13.8%, p=0.038), while PIK3CA mutations were significantly more frequent (28.1% vs 12.2%, p<0.001). TP53 remained the most common mutation overall (62%).
TCGA analysis confirmed enrichment of PIK3CA mutations in HER2-low TNBC and fewer BRCA2/HRR mutations compared with HER2-zero tumors.
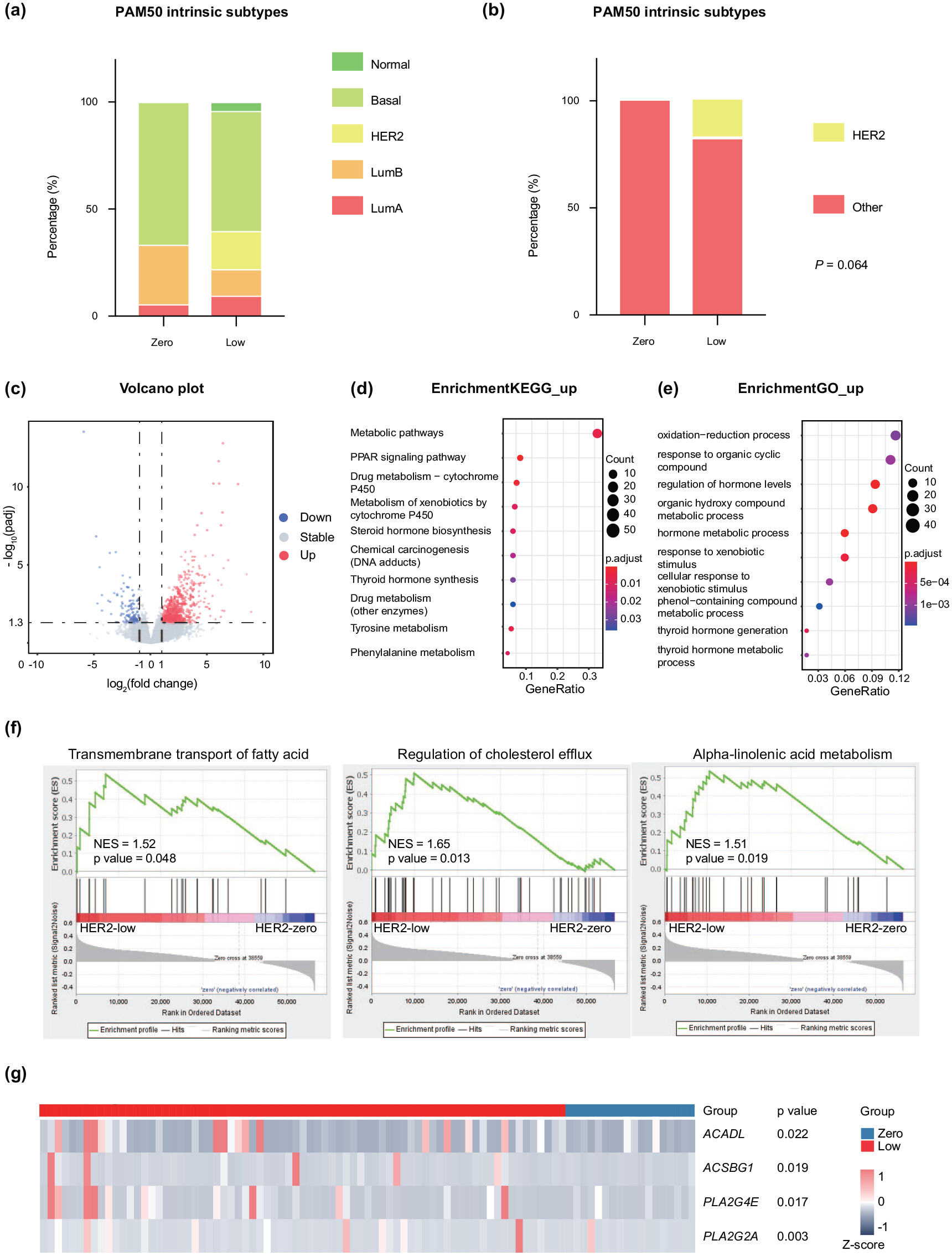
Transcriptomic Findings
HER2-low TNBC demonstrated a higher proportion of HER2-enriched (HER2-E) molecular subtype (17.8% vs 0.0%). Differentially expressed genes (n=375 upregulated, n=43 downregulated) were enriched in metabolic pathways, particularly lipid metabolism and fatty acid transport. Key genes such as ACADL and ACSBG1 suggested activation of fatty acid degradation, while PLA2G4E and PLA2G2A indicated enhanced α-linolenic acid metabolism.
Treatment Response
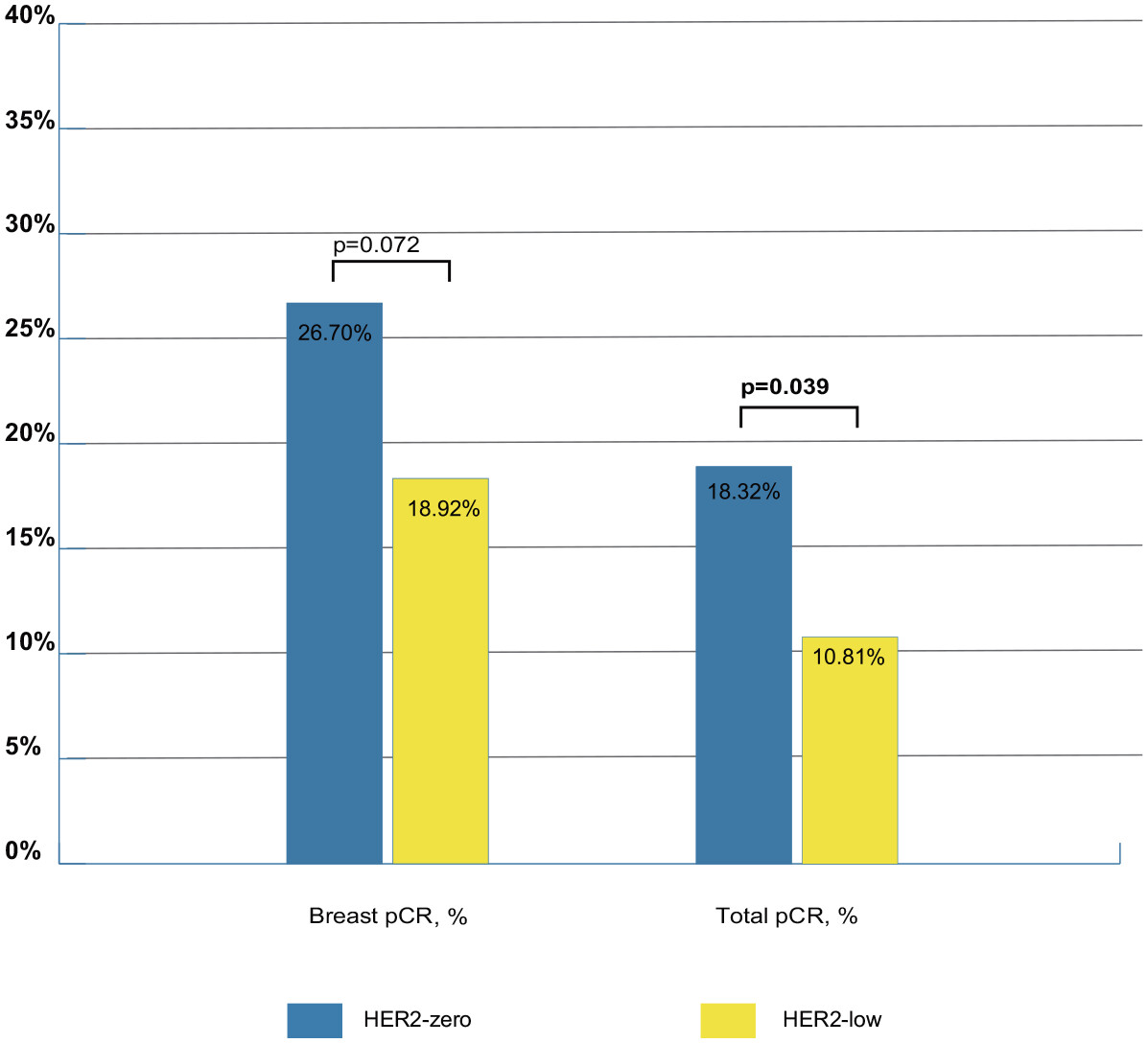
Among 376 patients receiving NAC, breast pCR and total pCR rates were 22.9% and 14.6%, respectively. HER2-zero tumors achieved higher total pCR than HER2-low tumors (18.3% vs 10.8%, p=0.039). Breast pCR rates did not significantly differ (26.7% vs 18.9%, p=0.072). Carboplatin improved pCR in univariate analysis, but this effect was not significant in multivariate models.
Survival Outcomes
With a median follow-up of 49.4 months, no survival differences were observed between HER2-low and HER2-zero groups:
- Breast cancer-free interval (HR=0.97; 95% CI: 0.79–1.20; p=0.796)
- Overall survival (HR=1.27; 95% CI: 0.95–1.68; p=0.10)
Independent predictors of worse outcomes included tumor size >2 cm, lymph node positivity, grade III, lymphovascular invasion, and non-standard adjuvant therapy.
Key Findings
- Nearly half of Asian TNBC patients were HER2-low.
- HER2-low TNBC was linked to postmenopausal status, invasive ductal histology, lymph node involvement, and more family history of breast/ovarian cancer.
- HER2-low tumors showed fewer BRCA1/2 mutations but significantly more PIK3CA mutations.
- Transcriptomic data indicated activation of lipid metabolism pathways in HER2-low tumors.
- HER2 status did not independently influence prognosis, but HER2-low tumors had lower total pCR rates following NAC.
Takeaway Messages
This study demonstrates that HER2-low TNBC is a biologically distinct entity, marked by metabolic pathway activation and enrichment of PIK3CA mutations, but without a clear survival disadvantage compared with HER2-zero TNBC. These findings reinforce the need for novel targeted therapies, particularly ADCs and PI3K inhibitors, to improve outcomes for this patient subgroup.
Conclusion
HER2-low TNBC accounts for nearly half of TNBC cases in Asian women and exhibits unique clinicopathologic and genomic features compared with HER2-zero tumors. While survival and chemotherapy response rates remain similar, the higher prevalence of PIK3CA mutations and metabolic pathway activation suggest promising avenues for targeted therapy development. Future prospective trials are warranted to evaluate HER2-low–specific treatment strategies, including ADCs and PI3K inhibitors, in TNBC.
You can read the full article here.
Written by Sona Karamyan, MD