
Rectal Cancer in Adults: What patients should know about
What is Rectal Cancer?
Rectal cancer is a type of cancer that forms in the tissues of the rectum. The rectum is part of the body’s digestive system. The digestive system takes in nutrients from foods and helps pass waste material out of the body. The digestive system is made up of the esophagus, stomach, and small and large intestines. The colon is the main part of the large intestine and is about 5 feet (1.5 meters) long. Together, the rectum and anal canal make up the last part of the large intestine and are 6 to 8 inches ( long. The anal canal ends at the anus (the opening of the large intestine to the outside of the body).
In this video, Stanford’s colon cancer experts explain that colon cancer is highly preventable through regular screening, and advancements in detection and treatment have significantly improved outcomes even for advanced disease.
Prevalence and Epidemiology
Rectal cancer is the third most common cancer in both men and women in the United States, with an estimated 106,590 new cases of colon cancer and 46,220 new cases of rectal cancer in 2024. The prevalence of rectal cancer varies by age, with the highest incidence occurring in individuals over the age of 50. The lifetime risk of developing colorectal cancer is about 1 in 23 for men and 1 in 25 for women. However, the incidence rate has been increasing in people under the age of 55, with rates increasing by 1% to 2% per year since the mid-1990s.
Causes and Risk Factors
The causes and risk factors of rectal cancer are multifactorial and can be influenced by both genetic and environmental factors. Some of the known risk factors include:
Inherited disorders: Certain inherited disorders, such as Lynch syndrome and familial adenomatous polyposis, can significantly increase the risk of developing rectal cancer.
Personal and family history of colorectal cancer: A personal or family history of colorectal cancer can raise the risk of developing rectal cancer.
Genetics: Specific genetic mutations, such as hereditary nonpolyposis colorectal cancer (HNPCC) or Lynch syndrome, can increase the risk of rectal cancer.
Radiation therapy: Previous radiation treatment to the abdomen can increase the risk of rectal cancer.
Other conditions: Conditions such as ovarian cancer, polyps, inflammatory bowel disease, obesity, type 2 diabetes, and a lack of exercise can also increase the risk of rectal cancer.
It is essential to note that while these factors can increase the risk of rectal cancer, they do not guarantee its development. Additionally, some lifestyle factors, such as a diet high in red, processed, or charred meats, smoking, and excessive alcohol consumption, can also contribute to the risk of developing rectal cancer.
Colorectal cancer risk factors. The image is taken from frontiersin.org
Symptoms
The symptoms of rectal cancer can vary depending on the stage and location of the tumor. Some common symptoms include:
- Changes in bowel habits
- Rectal bleeding or blood in the stool
- Abdominal pain or cramping
- Persistent urge to have a bowel movement
- Unexplained weakness and fatigue
- Unintended weight loss
- Anemia
It is essential to note that these symptoms can also be indicative of other conditions, so it is crucial to consult a healthcare professional for proper diagnosis.
Types and Diagnosis
The diagnosis and classification of rectal cancer involve several types of tests and procedures, as well as different types of cancer.
Types of Rectal Cancer
Adenocarcinoma: The most common type of rectal cancer, which develops in the glandular cells that line the inner surface of the rectum.
Small cell carcinomas: These start in the neuroendocrine cells that line the small intestine and are more common in the lungs but can also develop in the digestive tract.
Squamous cell carcinomas: These develop in the outer layer of the digestive tract and may be triggered by chronic inflammatory conditions and gastrointestinal tract infections.
Melanomas: These develop in the skin cells and are less common, with almost all cases forming in the skin around the anus.
Diagnosis of Rectal Cancer
Physical examination: A digital rectal exam is performed to assess the rectum and feel for any abnormalities.
Imaging tests: Computed tomography (CT) scans and magnetic resonance imaging (MRI) of the chest, abdomen, and pelvis are used to rule out metastatic disease and determine tumor extension and node status.
Endoscopy: Colonoscopy or flexible sigmoidoscopy is used to examine the rectum and colon, measure the distance from the lesion to the anal verge, and obtain tissue biopsies for pathological confirmation of rectal cancer.
Blood tests: Complete blood count and chemistry panel are performed to assess red blood cell count and organ function, while carcinoembryonic antigen testing may be used to monitor the response to treatment.
Staging
Stage I: Tumor is localized and has not invaded the muscularis propria.
Stage II: Locally advanced tumor that can be treated by chemotherapy, radiation, or surgery.
Stage III: Locally advanced tumor that can be treated by chemotherapy, radiation, or surgery.
Stage IV: Tumor has metastasized and is no longer confined to the rectum.
The specific criteria for Stages II and III can vary depending on the specific type of cancer.
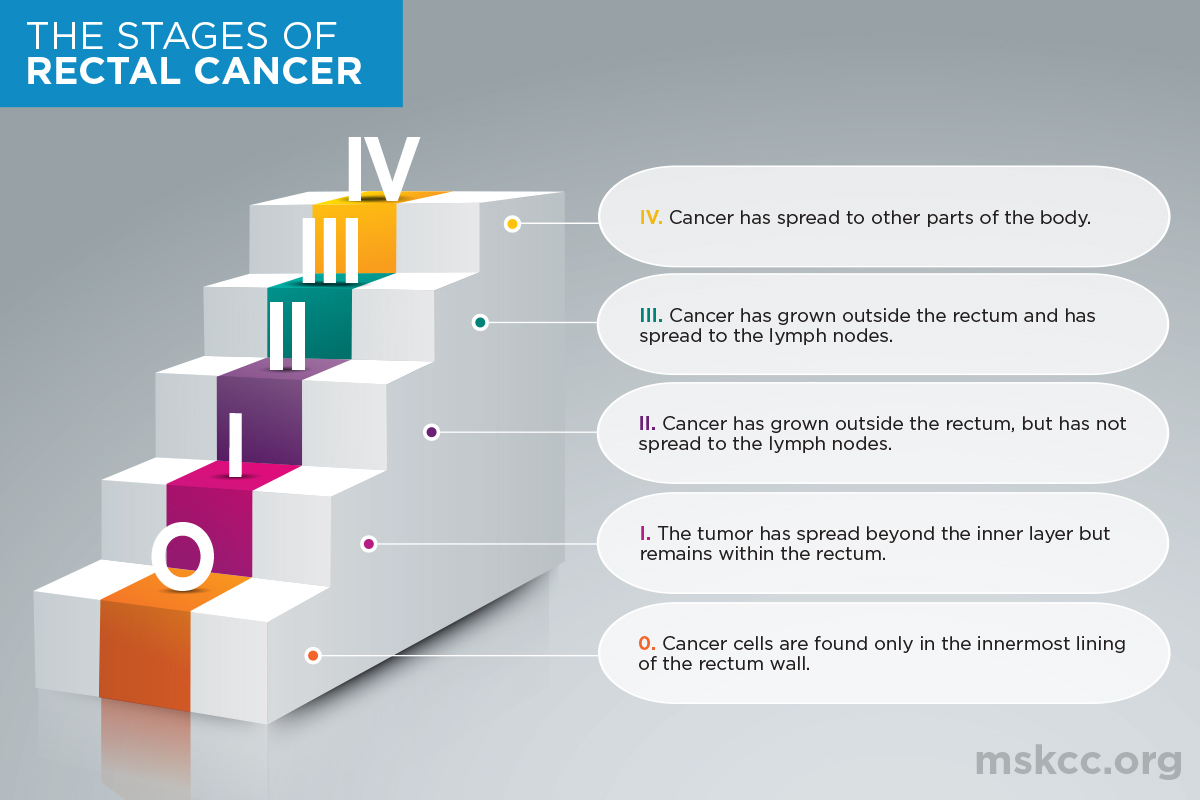
Rectal cancer stages. This image is taken from mskcc.org.
Treatment
The treatment of rectal cancer involves a combination of surgery, radiation therapy, chemotherapy, and targeted therapy, with a specific approach depending on the stage and location of the cancer, as well as the patient’s overall health and preferences. The latest approaches in rectal cancer treatment include:
- Neoadjuvant therapy: This involves the use of chemotherapy and radiation therapy before surgery to reduce the size of the tumor and improve the chances of successful surgery.
- Intensity-modulated radiation therapy (IMRT): IMRT is a type of radiation therapy that uses linear accelerators to deliver precise radiation to the tumor while minimizing exposure to nearby healthy tissues, potentially reducing adverse effects and improving tolerability.
- Immunotherapy: Immune checkpoint inhibitors, chimeric antigen receptor (CAR) T cell therapy, T cell receptor (TCR) alterations, and cytokine therapy are emerging treatments for colorectal cancer, including rectal cancer.
- Chemotherapy: Chemotherapy remains a mainstay of colorectal cancer treatment, with studies showing that it has increased the overall survival time of patients, particularly those with metastases, to approximately 20 months.
- Targeted therapy: Molecular targeted therapy is an emerging approach that aims to target specific proteins or pathways in cancer cells, potentially improving treatment efficacy and reducing side effects.
In this video patients diagnosed with colon cancer share their experiences with treatment.
Prognosis and Survival
The prognosis for rectal cancer depends on various factors, such as the stage of the cancer, the effectiveness of treatment, and the patient’s overall health. According to the American Cancer Society, the 5-year relative survival rate for colorectal cancer, which includes rectal cancer, is 65.1%. However, for patients diagnosed with localized rectal cancer, the 5-year survival rate can be as high as 91%.
For advanced and metastatic rectal cancer, the prognosis is generally poor. The median survival for patients with advanced non-resectable and metastatic rectal cancer is between 24 and 36 months. However, a subset of patients with best supportive care can have a median overall survival of 5 to 6 months.
In addition to the factors mentioned above, the prognosis for rectal cancer can also be influenced by factors such as the patient’s age, overall health, and the presence of any comorbidities. Patients need to discuss their prognosis with their healthcare team, as it can help them make informed decisions about their treatment and care.
Patient’s Survivorship
Rectal cancer survivorship involves understanding the causes of death and optimizing healthcare management. The 5-year survival rate for rectal cancer is 73.8%, and it decreases to 50.1% when the cancer has metastasized. Survivorship care includes cancer surveillance recommendations based on the NCCN guidelines and the use of total neoadjuvant therapy for curative treatment of locoregional rectal cancer. Patients may face a range of problems or side effects during and after treatment, which require careful management and follow-up, including managing long-term toxicity and addressing stressors such as fear of recurrence or death, social support, employment issues, and insurance concerns.
Problems During Treatment
During the treatment of rectal cancer, patients may face several challenges. These challenges can be physical, emotional, and social. Some of the common challenges include:
Side effects from treatment: Patients may experience side effects such as nausea, vomiting, fatigue, hair loss, and pain. To manage these side effects, patients should discuss potential side effects with their healthcare team and ask for appropriate medications or interventions to manage them.
Changes in bowel habits: Treatment may cause changes in bowel habits, such as diarrhea, constipation, or urgency, which can lead to discomfort and inconvenience. Patients should discuss their bowel habits with their healthcare team and seek advice on how to manage any issues.
Emotional and psychological issues: The diagnosis and treatment of rectal cancer can be emotionally and psychologically challenging for patients, affecting their quality of life and well-being. Patients should consider seeking support from mental health professionals, support groups, or counseling services to help manage any emotional or psychological challenges they may be facing.
Financial burden: The cost of cancer treatment, including medications, hospital stays, and follow-up appointments, can be a significant financial burden for patients and their families. Patients should discuss their financial concerns with their healthcare team and explore options for financial assistance, such as grants, support from organizations, or government programs. Patients may need to explore cost-sharing strategies, such as negotiating with healthcare providers, using generic medications, or seeking more affordable alternative treatment options
After treatment
Some of the common challenges include:
Bowel dysfunction: Patients may experience changes in bowel habits, such as diarrhea, constipation, or urgency, which can lead to discomfort and inconvenience.
Ostomy management: Patients with ostomies may face challenges related to the time and effort required for ostomy care and problems with ostomy equipment that could result in leaks.
Negative psychosocial effects: Some patients may experience fear and anxiety regarding gas, odor, incontinence, or leakage of stool or ostomy bag contents; not returning to “normal” after cancer; constraints on valued activities; relationship and intimacy problems; and other emotional and mental health issues beyond bowel function.
Late effects of cancer treatments: Survivors may experience hernias, bowel obstruction or blockage, urinary incontinence and fistulas, fatigue, concentration, and stamina problems, and enduring pain and discomfort.
Comorbidities and aging: Older patients or those with pre-existing conditions may face challenges related to aging or specific conditions, such as arthritis, heart disease, or other cancers.
It is essential for patients to discuss these challenges with their healthcare team and to develop a comprehensive treatment plan that addresses their individual needs and concerns. Support groups and counseling services can also help patients cope with the emotional and psychological aspects of their treatment.
Recommendations for Patients
Understand your diagnosis: Learn about the different stages of rectal cancer and the treatment options available for each stage. This will help you make informed decisions about your care and discuss your options with your healthcare team.
Seek support: Connect with other patients, support groups, and healthcare professionals who can provide emotional and practical support during your treatment journey.
Prepare for appointments: Before meeting with your healthcare team, gather information about your diagnosis, treatment options, and any concerns or questions you may have. This will help you make the most of your appointments and ensure you receive the best possible care.
Follow treatment guidelines: Adhere to your treatment plan, which may include surgery, radiation therapy, chemotherapy, or a combination of these treatments. Your healthcare team will provide detailed instructions on preparing for and recovering from each treatment.
Manage side effects: Be aware of potential side effects from your treatment, such as nausea, vomiting, fatigue, hair loss, and pain. Discuss these side effects with your healthcare team and ask for appropriate medications or interventions to manage them.
Consider clinical trials: Ask your healthcare team about participating in clinical trials testing new treatments, interventions, and tests as a means to prevent, detect, treat, or manage rectal cancer.
Cope with the emotional impact: A diagnosis of rectal cancer can be overwhelming. Seek support from friends, family, and healthcare professionals to help you cope with the distress and uncertainty of cancer.
Stay informed: Learn about rectal cancer and its treatment options to make informed decisions about your care. Ask your doctor about your cancer, including your treatment options and, if you like, your prognosis.
Prepare for surgery: If you are undergoing surgery, follow your healthcare team’s instructions for bowel preparation and discuss any concerns you may have.
Consider palliative care: Palliative care can provide relief from pain and other symptoms of a severe illness. It is offered alongside curative or other treatments you may be receiving.
Listen to Kelly’s moving story about his illness.
Conclusion
While the journey with rectal cancer can be challenging, it is crucial to remember that progress and hope are within reach. With the support of loved ones, healthcare professionals, and the advancements in medical research, patients can overcome challenges and find hope in the face of adversity. By staying informed, adhering to treatment plans, and participating in clinical trials, patients can contribute to the ongoing efforts to improve the management and outcomes of rectal cancer. Together, we can work towards a brighter future for those affected by this disease.
Resources
- Clinicaltrials.gov
- National Cancer Institute – cancer.gov
- American Cancer Society – cancer.org
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Canadian Cancer Society – cancer.ca
- Memorial Sloan Kettering Cancer Center – mskcc.org
- City of Hope – CancerCenter.com
- John Hopkins Medicine – hopkinsmedicine.org
- Colorectal cancer Alliance – Colorectalcancer.org
- Long-term survival of a patient with advanced rectal cancer and multiple pelvic recurrences after seven surgeries – PubMed
- Rectal Cancer – PubMed
- Yale Medicine – yalemedicine.org
- ASCO Publications – ascopubs.org
- Becker’s GI and Endoscopy – beckersasc.com
- Greatest Challenges of Rectal Cancer Survivors: Results of a Population-Based Survey – PubMed
- Oncodaily.com
