Male Breast Cancer: What patients should know about
What is Male breast cancer ?
Male breast cancer is a rare cancer that develops in the breast tissue of men. It begins when cells in the breast tissue undergo malignant changes and start to grow uncontrollably, forming a tumor. This type of cancer can occur in the small amount of breast tissue that all individuals, regardless of gender, are born with.
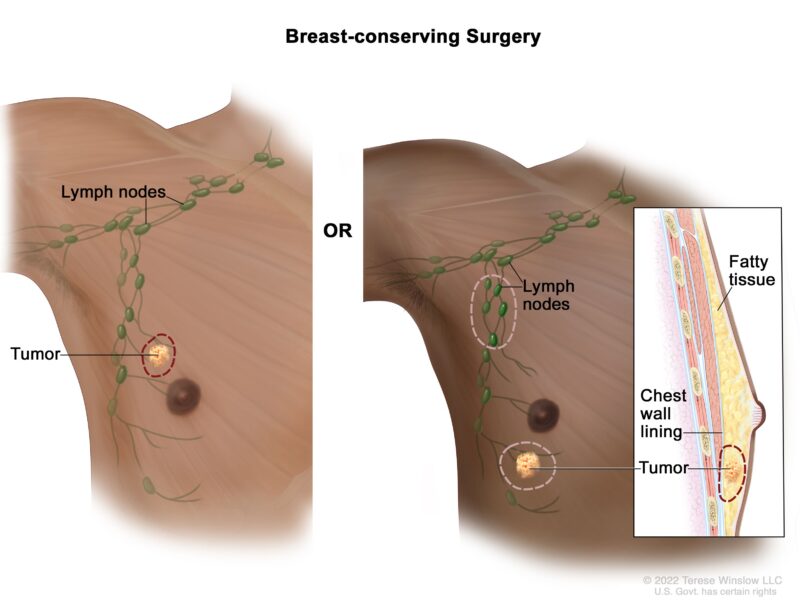
This image is taken from “The National Cancer Institute”.
Epidemiology
The epidemiology of male breast cancer highlights its rarity and the trends in incidence and mortality over time.
- Male breast cancer is relatively rare, accounting for less than 1% of all breast cancer cases.
- The incidence of male breast cancer has been increasing over the years. From 2004 to 2014, the incidence rose from 7.2% to 10.3%.
- In 2023, it is estimated that about 2,800 men in the United States will be diagnosed with breast cancer.
- Black men have the highest incidence rates of breast cancer among men, followed by White men.
Causes and Risk Factors
Male breast cancer can be influenced by several risk factors:
- Genetic Factors: Mutations in genes such as BRCA1 and BRCA2 can increase the risk.
- Age: The majority of male breast cancer cases are diagnosed in men over 50 years old.
- Family History: Having close relatives with breast cancer increases risk.
- Hormonal Factors: Conditions that increase estrogen levels, such as obesity or liver disease, can contribute to risk.
- Radiation Exposure: Previous radiation treatment to the chest area is a known risk factor.
Signs and Symptoms
Male breast cancer, though less common than female breast cancer, presents with a variety of symptoms that are important for early detection and diagnosis. Here are the symptoms associated with male breast cancer:
Common symptoms
1. Lump or Mass in the Breast: The most frequently reported symptom of male breast cancer is a lump or mass in the breast, often painless, which may be felt as a hard knot or pebble-like structure. This lump is typically located beneath the nipple and areola but can also occur anywhere in the breast tissue.
2. Nipple Changes:
- Nipple Discharge: Nipple discharge, particularly if it is bloody or clear, is a significant symptom that can indicate male breast cancer. While nipple discharge can also be benign, its presence warrants further investigation.
- Inversion or Retraction: A nipple turning inward or appearing retracted is another common symptom.
- Rash or Ulceration: Changes around the nipple, including rashes, scaling, or the appearance of sores or ulcers, can be indicative of male breast cancer.
3. Skin Changes:
- Dimpling or Puckering: The skin over the breast may show dimpling or puckering, similar to the texture of an orange peel.
- Redness or Swelling: Parts of the breast may appear red, swollen, or inflamed.
Less Common Symptoms
4. Changes in Breast Size or Shape: Any alteration in the size or shape of the breast or chest area, particularly if it is unilateral (on one side only), should be promptly evaluated.
5. Lymph Node Changes: Swelling or enlargement of lymph nodes in the armpits, collarbone, or neck can occur if the cancer has spread to these areas. This symptom is particularly concerning and warrants immediate medical attention.

The image is taken from the “We Get It Too” Inc.
Diagnosis
1. Initial Evaluation
The first step in diagnosing male breast cancer is a physical exam by a doctor to check for lumps, changes in the skin or nipple, or nipple discharge. The doctor will also take a medical history to assess risk factors like family history, genetic predispositions, and previous radiation exposure.
2. Imaging Tests
If a suspicious lump or other signs are found, imaging tests are ordered:
- Mammography: Despite being less common in men, mammography is used to detect abnormalities in male breast tissue. It can show lumps, masses, and calcifications that are not palpable on physical exam. During a mammogram, the breasts are compressed between two plates to flatten the tissue and make masses easier to identify.
- Ultrasound: Ultrasound uses sound waves to create images of the breast tissue. It can help determine if a mass found on mammogram or physical exam is solid or fluid-filled (a cyst).
- MRI: Breast MRI may be used in some cases to further evaluate a suspicious area.
3. Biopsy
If imaging tests reveal a suspicious area, a biopsy is performed to obtain a sample of the tissue for analysis under a microscope. This is the definitive way to diagnose breast cancer.
- Core needle biopsy: A hollow needle is used to remove a small cylinder of tissue from the mass. This can be done with imaging guidance.
- Fine needle aspiration: A thin needle is used to remove fluid and/or cells from a cyst or mass.
The tissue sample is examined by a pathologist to determine if cancer is present and what type it is. The pathologist also tests the tumor for estrogen, progesterone, and HER2 receptors, which helps guide treatment.
4. Staging Tests
If male breast cancer is diagnosed, additional tests may be done to determine the stage and extent of disease:
- Bone scan: To check for spread to the bones
- CT scan: To look for spread to the chest, abdomen or pelvis
- PET scan: To check for spread to lymph nodes or other organs
The stage, from 0 to IV, reflects the tumor size and whether it has spread to lymph nodes or other organs. This information helps guide treatment planning. Early diagnosis is key for the best outcomes in male breast cancer. Men should promptly report any breast changes to their doctor.
Watch this short informative video from “The University of Mississippi Medical Center” about Early Detection of Male Breast Cancer.
Treatment of Male Breast Cancer
1. Surgery
- Mastectomy – This is the most common procedure, which involves removing the entire breast. This is usually the only surgery needed for early-stage cancers.
- Lumpectomy – In some cases, a lumpectomy may be an option if the tumor is small and has not spread. A lumpectomy removes just the tumor and a small amount of surrounding healthy tissue. This is usually followed by radiation therapy to the breast.
- Lymph nodes in the armpit area may also be removed, either during the mastectomy or as a separate procedure, to check for cancer spread. This is called a sentinel lymph node biopsy or axillary lymph node dissection.
2. Radiation Therapy
Radiation uses high-energy beams to kill cancer cells. It may be given after surgery, especially if a lumpectomy was done, to kill any remaining cancer cells. Radiation is often aimed at the chest wall and lymph nodes in the armpit.
3. Hormone Therapy
- Over 90% of male breast cancers are estrogen receptor-positive, so hormone therapy is commonly used. This means the cancer cells have receptors that allow them to use the hormone estrogen to grow and spread. Hormone therapy is commonly used to block or lower estrogen levels and prevent recurrence.
- Tamoxifen is the most common hormone therapy drug for men. It works by blocking estrogen from attaching to and fueling cancer cells. Tamoxifen is usually taken daily for 5-10 years after surgery.
- Hormone therapy may be given after surgery to reduce recurrence risk or for advanced disease to slow progression.
4. Targeted Therapy
Targeted drugs attack specific molecules involved in cancer growth. They may be used after surgery or for advanced disease. They are usually given in combination with hormone therapy or chemotherapy. The role of HER2-targeted therapy is still being studied in male breast cancer, as HER2-positivity is less common compared to female breast cancer. However, if a tumor tests positive for HER2, drugs like trastuzumab may be used.
5. Chemotherapy
Chemotherapy uses anti-cancer drugs that are given intravenously or as pills. These drugs travel through the bloodstream to kill rapidly dividing cancer cells throughout the body. Chemotherapy may be given before surgery to shrink a tumor and make it easier to remove. It can also be given after surgery to kill any remaining cancer cells and reduce the risk of recurrence. Chemotherapy is also an option for advanced or recurrent breast cancer. The specific chemodrugs used depend on factors like the cancer’s characteristics and the man’s overall health.
Watch this short video from “Baylor Scott and White Health”, where a patient with male breast cancer shares his story.
Side Effects of Chemotherapy
Fatigue
Fatigue is the most common side effect of chemotherapy. It can cause to feel extremely tired and lacking in energy, even after resting. Coping strategies include getting plenty of rest, doing light exercise if possible, and asking for help with daily tasks.
Hair Loss
Many chemotherapy drugs can cause hair loss (alopecia) from all over the body, including the head, face, arms and legs. Hair loss usually starts a few weeks after beginning treatment and increases over time. Hair typically grows back after treatment ends.
Nausea and Vomiting
Chemotherapy can cause nausea and vomiting, which can range from mild to severe. Anti-nausea medications are usually given before and after treatment to prevent or control this Staying hydrated and eating small, frequent meals may help.
Mouth Sores
Chemotherapy can damage the cells lining the mouth and throat, causing painful mouth sores (mucositis). This usually occurs 5-14 days after treatment. Keeping the mouth clean and eating soft, bland foods can help. Mouth sores typically heal after treatment ends.
Diarrhea or Constipation
Chemotherapy can cause either diarrhea or constipation. Diarrhea leads to loose, watery stools, while constipation causes difficulty having bowel movements. Medications and dietary changes may help regulate bowel function.
Increased Infection Risk
Chemotherapy can lower white blood cell counts, increasing the risk of infection. Signs of infection include fever, chills, sore throat, and redness/swelling at IV sites. Prompt treatment with antibiotics is important.
Anemia
Chemotherapy can cause anemia by lowering red blood cell counts. Symptoms include fatigue, dizziness, and shortness of breath. Iron supplements or blood transfusions may be needed in severe cases.
Nerve Damage
Some chemotherapy drugs can cause peripheral neuropathy, leading to numbness, tingling, weakness or pain in the hands and feet. This is usually temporary but can be permanent in some cases. Most side effects gradually improve after treatment ends. Medications, dietary changes, and other supportive care measures can help manage many side effects. It’s important to report any side effects to your doctor so they can be properly treated.
Treatment is tailored to the individual based on factors like cancer stage, receptor status, age, and overall health. A multidisciplinary team develops the treatment plan. Early diagnosis is key to the best outcomes.
Prognosis and Survival
- The 5-year relative survival rate for male breast cancer in the U.S. is 82%. If the cancer is localized to the breast, the 5-year survival rate is 95%.
- However, men with breast cancer have a higher mortality rate compared to women, especially in the first 5 years after diagnosis. The 5-year overall survival rate was 77.6% for men vs 86.4% for women in one study.
- Factors contributing to the survival disparity include a later stage at diagnosis, more aggressive tumor characteristics, and undertreatment in men compared to women. Men are less likely to receive radiation therapy, especially after breast-conserving surgery.
The prognosis for male breast cancer has improved over time, but more research is still needed to understand the unique factors affecting outcomes in men. Early diagnosis and prompt treatment are crucial for the best chances of survival. Men diagnosed with breast cancer should discuss their individual prognosis and treatment options with their oncology team.
Follow-up Care and recommendations for patients
- Regular Check-ups with the cancer care team 1-4 times per year for the first 5 years after treatment, and then once a year after that.
- Screening tests like mammograms may be recommended, even though male breast cancer is rare. An annual mammogram of the affected breast should be offered if possible.
- It’s important to receive a treatment summary and survivorship care plan to share with your other doctors.
- Cancer rehabilitation services like physical therapy, counseling, and support groups can help with the physical and emotional effects of male breast cancer.
- Maintaining a healthy lifestyle with proper nutrition, exercise, and stress management can also support your recovery.
In summary, regular follow-up care is essential for male breast cancer survivors to ensure the best possible long-term outcomes. Be sure to discuss your specific follow-up plan with your oncology team.
Resources
- Compass Oncology – compassoncology.com
- Male breast cancer presenting as nipple discharge, Prognostic Factors in Male Breast Cancer – PubMed
- American Cancer Society – cancer.org
- Cancer Research UK – cancerresearchuk.org
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Penn Medicine Abramson Cancer Center – pennmedicine.org
- National Cancer Institute – cancer.gov
- Johns Hopkins Medicine – hopkinsmedicine.org
- Canadian Cancer Society – cancer.ca
- National Breast Cancer Foundation provides early detection screenings, including mammograms, breast health education, and a supportive community – nbcf.org
- Oncodaily.com – Online platform where you can find anything related to cancer such as everyday news, blogs, videos, podcasts, etc.
- Stanford Medicine – med.stanford.edu
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023