Burkitt Lymphoma: What patients should know about
What is Burkitt Lymphoma?
Burkitt lymphoma is a highly aggressive form of B-cell non-Hodgkin lymphoma. It is characterized by the rapid growth of tumors and is considered one of the fastest-growing human tumors.
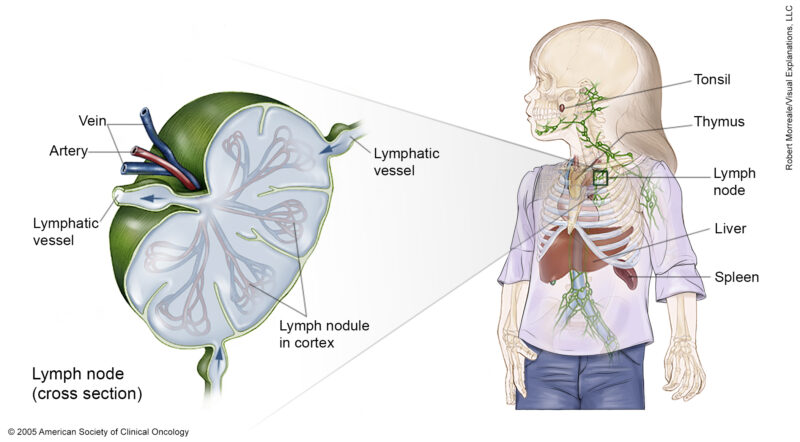
Source of image cancer.net
Types of Burkitt Lymphoma
Endemic Burkitt Lymphoma:
- Predominantly found in equatorial Africa and Papua New Guinea.
- Commonly affects children aged 4 to 7.
- Often associated with Epstein-Barr virus (EBV) and malaria.
- Typically presents with tumors in the jaw or facial bones.
Sporadic Burkitt Lymphoma:
- Occurs worldwide, including North America and Europe.
- More common in children and young adults.
- Frequently presents with abdominal tumors, particularly in the ileocecal region.
- Less commonly associated with EBV compared to the endemic form.
Immunodeficiency-Related Burkitt Lymphoma:
- Occurs in individuals with compromised immune systems, such as those with HIV/AIDS or organ transplant recipients.
- Considered an AIDS-defining cancer.
- It can present with generalized and bulky disease, often involving the liver, spleen, and bone marrow.
Causes and Risk Factors
Burkitt lymphoma (BL) is a rare and aggressive form of non-Hodgkin lymphoma that primarily affects B-cells. The exact causes of Burkitt lymphoma are not fully understood, but several factors have been identified that may increase the risk of developing this disease. These factors can be broadly categorized into causes and risk factors.
Causes
Epstein-Barr Virus (EBV):
- EBV is strongly associated with Burkitt lymphoma, particularly the endemic form found in Africa. The virus is known to cause infectious mononucleosis and is present in nearly all cases of endemic Burkitt lymphoma.
- In sporadic and immunodeficiency-related forms, the association with EBV is less pronounced but still significant.
Chromosomal Translocations:
- The genetic mutation is a critical factor in the development of the disease.
Malaria:
- Chronic malaria infection is a significant cause of endemic Burkitt lymphoma. Malaria is thought to weaken the immune system, allowing EBV to transform infected B-cells into cancerous cells.
HIV/AIDS:
- Immunodeficiency-related Burkitt lymphoma is commonly seen in individuals with HIV/AIDS. The weakened immune system in these patients increases the risk of developing this type of lymphoma.
Risk Factors
Immunodeficiency:
- Conditions that weaken the immune system, such as HIV/AIDS or the use of immunosuppressive drugs (e.g., post-organ transplantation), increase the risk of developing Burkitt lymphoma.
Age and Gender:
- Burkitt lymphoma is more common in children, particularly boys aged 5 to 10 years, in endemic regions. In non-endemic regions, it can affect both children and adults, with a higher incidence in males.
Geographic Location:
- Endemic Burkitt lymphoma is most prevalent in equatorial Africa and Papua New Guinea, where malaria is common. Sporadic cases are more frequent in North America and Europe.
Previous Infections:
- Prior infections with EBV and hepatitis have been identified as risk factors. For instance, hepatitis infection has been associated with an increased risk of Burkitt lymphoma in older adults.
Lifestyle Factors:
- Smoking and alcohol consumption have been studied as potential risk factors. Interestingly, some studies have found an inverse association between smoking and the risk of Burkitt lymphoma, though the reasons for this are not well understood.
Genetic Susceptibility:
- Genetic predispositions, such as inherited immune deficiencies, can also increase the risk of developing Burkitt lymphoma.
Summary
While the exact causes of Burkitt lymphoma are not fully understood, several factors have been identified that contribute to the risk of developing this aggressive cancer. These include viral infections (EBV, HIV), genetic mutations (MYC translocation), chronic infections (malaria), and immunodeficiency. Understanding these causes and risk factors is crucial for early diagnosis and effective treatment of Burkitt lymphoma.
Symptoms
General Symptoms
- Swollen Lymph Nodes: Painless swellings in the neck, armpit, groin, or other areas due to enlarged lymph nodes.
- B Symptoms: Fever, drenching night sweats, and unexplained weight loss. These symptoms often occur together and are known as ”B symptoms”.
- Fatigue and Weakness: General tiredness and a feeling of weakness.
- Loss of Appetite: Reduced desire to eat, which can contribute to weight loss.
Symptoms Based on Disease Location
Abdominal Symptoms (common in sporadic Burkitt lymphoma):
- Abdominal Pain: Pain in the abdomen or back.
- Swelling: Swelling of the abdomen due to fluid accumulation (ascites).
- Nausea and Vomiting: Feeling sick or being sick.
- Diarrhea: Frequent loose or watery stools.
- Bowel Obstruction: Pain and symptoms related to a blockage in the bowel.
Facial and Jaw Symptoms (common in endemic Burkitt lymphoma):
- Swelling and Distortion of Facial Bones: Enlargement of the jaw or other facial bones.
- Rapid Growth of Lymph Nodes: Non-tender, rapidly enlarging lymph nodes in the facial area.
Bone Marrow Involvement:
- Anemia: Shortage of red blood cells, causing tiredness and shortness of breath.
- Thrombocytopenia: Shortage of platelets, leading to easy bruising and bleeding.
- Neutropenia: Shortage of white blood cells, increasing the risk of infections.
Central Nervous System (CNS) Involvement:
- Headaches and Neurological Symptoms: Symptoms related to the brain and spinal cord, such as headaches, seizures, or changes in mental status.
Other Symptoms:
- Chest Pain: Pain in the chest, which can be due to lymphoma involvement in the chest area.
- Coughing or Trouble Breathing: Respiratory symptoms if the lymphoma affects the lungs or chest.
Diagnosis
Diagnosing Burkitt lymphoma (BL) involves a combination of clinical evaluation, imaging studies, laboratory tests, and histopathological examination. Given the aggressive nature of the disease, prompt and accurate diagnosis is crucial for effective treatment.
Clinical Evaluation
- Physical Examination: Initial assessment includes a thorough physical examination to check for signs such as rapidly growing masses, particularly in the abdomen, head, neck, or other areas.
Imaging Studies
- CT and PET Scans: Imaging studies such as CT scans and PET scans are essential for staging and identifying the extent of the disease. These scans help visualize the metabolic activity of the tumors and their spread to various body parts.
- MRI: MRI may be used, especially if there is suspicion of central nervous system (CNS) involvement.
Laboratory Tests
- Complete Blood Count (CBC): This test measures the levels of different blood cells. In Burkitt lymphoma, there may be an increased number of white blood cells and decreased numbers of red blood cells or platelets.
- Lactate Dehydrogenase (LDH): Elevated LDH levels are common in Burkitt lymphoma due to the high turnover rate of the tumor cells.
- Blood Chemistry Tests: These tests check for kidney and liver function and electrolyte imbalances, which can be affected by the disease and its treatment.
Histopathological Examination
- Biopsy: A definitive diagnosis is made through a biopsy of the affected tissue, such as an enlarged lymph node or bone marrow. The biopsy sample is examined under a microscope to identify the characteristic “starry-sky” pattern of Burkitt lymphoma, which includes a high mitotic rate and the presence of benign macrophages engulfing apoptotic malignant lymphocytes.

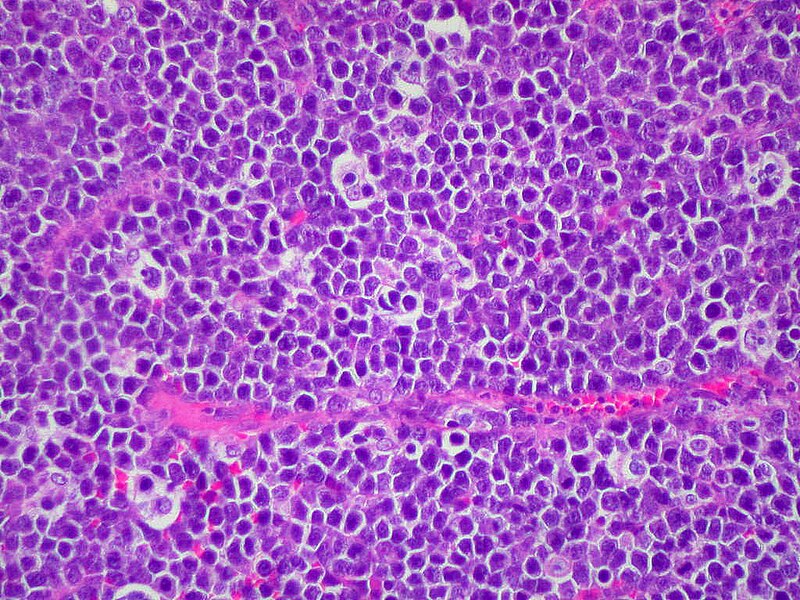
‘Starry Night’ by Vincent van Gogh and ‘Starry Sky’ of Burkitt Lymphoma – Source of images Wikimedia Commons
- Immunohistochemistry and Flow Cytometry: These tests are used to identify specific markers on the surface of the lymphoma cells. Burkitt lymphoma cells typically express surface immunoglobulin M (IgM) and B-cell markers, while being negative for T-cell markers and immature markers.
Cytogenetic and Molecular Studies
- Cytogenetic Analysis: This involves looking for specific genetic abnormalities, such as the translocation (when one gene from a chromosome jumps to another) of the MYC gene on chromosome 8 into 14, which is a hallmark of Burkitt lymphoma. Techniques like fluorescence in situ hybridization (FISH) and polymerase chain reaction (PCR) can detect these genetic changes.
Additional Tests
- Bone Marrow Biopsy: This test is performed to check for the involvement of the bone marrow, which is common in Burkitt lymphoma. The presence of lymphoma cells in the bone marrow has significant implications for treatment planning.
- Lumbar Puncture: A lumbar puncture is done to evaluate the cerebrospinal fluid (CSF) for lymphoma cells, especially if there are symptoms suggesting CNS involvement. Intrathecal chemotherapy may be administered during this procedure.
Treatment
Burkitt lymphoma (BL) is a highly aggressive form of non-Hodgkin lymphoma that requires prompt and intensive treatment. The primary treatment modality is chemotherapy, often combined with immunotherapy.
Chemotherapy
Chemotherapy is the cornerstone of treatment for Burkitt lymphoma. The regimens are intensive and typically involve multiple drugs. Common chemotherapy regimens include:
CODOX-M/IVAC:
- CODOX-M: Cyclophosphamide, doxorubicin, vincristine, and methotrexate.
- IVAC: Ifosfamide, etoposide, and cytarabine.
- This regimen is often used in combination with rituximab, a monoclonal antibody targeting B-cells.
HyperCVAD:
- Cyclophosphamide, vincristine, doxorubicin, and dexamethasone, alternating with high-dose methotrexate and cytarabine.
- Also typically combined with rituximab.
DA-EPOCH-R:
- Dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin, plus rituximab.
- This regimen is tailored to the patient’s tolerance and can be administered in an outpatient setting.
CALGB 1002 Protocol:
- An intensive regimen developed by the Cancer and Leukemia Group B, which includes multi-agent chemotherapy with rituximab.
- This protocol has shown high cure rates but is associated with significant toxicity.
Immunotherapy and Target Therapy
- Rituximab: A monoclonal antibody that targets B-cells, used in combination with chemotherapy to enhance treatment efficacy.
- CAR T-cell Therapy: Chimeric Antigen Receptor (CAR) T-cell therapy, is being explored for relapsed or refractory Burkitt lymphoma. This approach has shown promise in clinical trials.
Intrathecal Chemotherapy
Given the high risk of central nervous system (CNS) involvement, intrathecal chemotherapy (directly into the cerebrospinal fluid) is often administered. Drugs like methotrexate and cytarabine are commonly used for this purpose.
Stem Cell Transplantation
Autologous Stem Cell Transplantation: Involves high-dose chemotherapy followed by the infusion of the patient’s own stem cells. This is considered for patients who relapse or do not respond to initial treatment.
Supportive Care
- Tumor Lysis Syndrome (TLS) Management: Prophylactic measures such as hydration, allopurinol, or rasburicase are used to prevent TLS, a potentially life-threatening condition caused by the rapid breakdown of tumor cells.
- Growth Factors: Granulocyte-macrophage colony-stimulating factor (GM-CSF) or granulocyte colony-stimulating factor (G-CSF) may be used to support white blood cell counts during chemotherapy.
Prognosis and Survivorship
The prognosis for Burkitt lymphoma varies widely based on factors such as age, stage at diagnosis, response to treatment, and genetic factors. While children generally have a better prognosis than adults, intensive treatment can lead to long-term remission in many cases. Survivorship care is crucial for monitoring recurrence, managing late effects, and maintaining quality of life. Regular follow-up and a healthy lifestyle are key components of long-term survivorship for patients with Burkitt lymphoma.
Survivorship Challenges
Survivorship for Burkitt lymphoma patients involves navigating a range of challenges that can impact their quality of life long after treatment has ended. These challenges are multifaceted, encompassing physical, psychological, social, and practical aspects.
Watch George’s Cancer Survival Story from Texas Children’s Hospital
Physical Challenges
- Late Effects of Treatment: Many survivors experience long-term side effects from their treatments, such as chronic fatigue, cardiovascular issues, neuropathy, and secondary cancers. These late effects can persist for years and require ongoing management.
- Comorbidities: Older survivors often have other health conditions that complicate their recovery and overall health management.
Psychological Challenges
- Mental Health Issues: Survivors frequently face psychological distress, including anxiety, depression, and post-traumatic stress disorder (PTSD). These mental health issues can stem from the trauma of the cancer experience and the fear of recurrence.
- Existential Concerns: Many survivors struggle with existential issues such as finding meaning in life, coping with fear of recurrence, and dealing with feelings of grief and guilt.
Social and Practical Challenges
- Financial Toxicity: The economic burden of cancer treatment can be overwhelming, leading to financial stress due to medical expenses, lost wages, and reduced productivity. This financial strain can persist long after treatment ends.
- Employment Issues: Survivors may struggle to find or keep jobs due to ongoing health issues and the need for frequent medical appointments.
- Transportation and Accessibility: Rural survivors, in particular, face challenges related to transportation and access to healthcare services, which can hinder their ability to receive timely follow-up care and support.
Survivorship Care
- Lack of Survivorship Care Plans (SCPs): Many survivors are not provided with a comprehensive survivorship care plan, which outlines follow-up care and lifestyle recommendations. Even when SCPs are provided, there is often poor communication and support in implementing these plans.
- Coordination of Care: Effective communication and coordination between cancer care teams and primary care providers are often lacking, leading to fragmented care and unmet health needs.
During Treatment
Common Side Effects and Management Strategies
Fatigue
- Management: Regular light exercise, adequate rest, and balanced nutrition can help manage fatigue. Consulting with a healthcare provider for personalized advice is also beneficial.
Nausea and Vomiting
- Management: Anti-nausea medications (antiemetics) can be prescribed. Dietary adjustments, such as eating small, frequent meals and avoiding strong odors, can also help.
Diarrhea and Constipation
- Management: Medications like laxatives for constipation and anti-diarrheal drugs for diarrhea can be used. Staying hydrated and following dietary recommendations from healthcare providers is important.
Hair Loss
- Management: Hair loss is often temporary. Patients can use wigs, hats, or scarves to cope with this side effect. Psychological support may also be beneficial.
Peripheral Neuropathy
- Management: Medications to manage pain and discomfort, physical therapy, and lifestyle adjustments can help. It’s important to report symptoms to healthcare providers for appropriate interventions.
Infections
- Management: Preventive measures include maintaining good hygiene, avoiding crowds, and possibly using prophylactic antibiotics. Monitoring blood counts and seeking prompt medical attention for signs of infection is crucial.
Tumor Lysis Syndrome (TLS)
- Management: Preventive measures include hydration, medications like allopurinol or rasburicase, and close monitoring of kidney function and electrolytes.
Mouth Sores (Oral Mucositis)
- Management: Good oral hygiene, using mouth rinses, and avoiding spicy or acidic foods can help. Pain management strategies and nutritional support may also be necessary.
Loss of Appetite
- Management: Nutritional counseling, small frequent meals, and appetite stimulants can be used. Addressing underlying causes like nausea or mouth sores is also important.
Fertility Issues
- Management: Discussing fertility preservation options before starting treatment is crucial. Options may include sperm banking, egg or embryo freezing, and other assisted reproductive technologies.
Heart Problems
- Management: Regular monitoring of heart function, lifestyle modifications, and medications to manage heart conditions can be necessary. Early detection and intervention are key.
Bone Density Loss
- Management: Calcium and vitamin D supplements, weight-bearing exercises, and medications to strengthen bones may be recommended.
Supportive Care
Supportive care is an integral part of managing side effects. This includes:
- Psychological Support: Counseling, support groups, and mental health services can help patients cope with the emotional and psychological impact of cancer treatment.
- Nutritional Support: Dietitians can provide tailored advice to manage side effects like appetite loss and digestive issues.
- Physical Therapy: Helps manage fatigue, and neuropathy, and maintains physical function.
Effective management of side effects involves a multidisciplinary approach, including medications, lifestyle modifications, and supportive care services. Patients should maintain open communication with their healthcare team to address side effects promptly and effectively.
After Treatment
Follow-up Care
After treatment for Burkitt lymphoma, follow-up care is essential to monitor recovery, detect any signs of recurrence, manage side effects, and address any long-term health issues.
Frequency and Duration:
- Follow-up appointments are typically scheduled every 3 to 4 months during the first 2 to 3 years after treatment, and then less frequently.
- Most hospital teams offer follow-up for at least one year after treatment, after which the primary care physician often becomes the main point of contact.
Types of Follow-Up Care:
- Hospital-Based Follow-Up: Regular visits to the hospital where the treatment was received, involving physical exams, blood tests, and possibly scans if symptoms warrant it.
- GP and Community-Based Follow-Up: After the initial intensive follow-up period, care may transition to the patient’s GP, who will monitor for any health concerns and manage ongoing care.
- Telehealth: Some follow-up care can be conducted via telehealth, which is particularly useful for patients in rural or remote areas.
Monitoring and Tests
Physical Examinations and Tests:
- Regular physical exams and blood tests are common to check for signs of recurrence and monitor overall health.
- Imaging tests like PET/CT scans may be used initially to confirm remission but are less common unless symptoms suggest a recurrence.
Survivorship Care Plans:
- A survivorship care plan includes a summary of the treatment received, a schedule for follow-up visits, and recommendations for managing long-term side effects.
- This plan helps ensure continuity of care and provides a clear roadmap for both the patient and healthcare providers.
Managing Side Effects and Long-Term Health
Side Effects Management:
- Follow-up care involves managing both immediate and long-term side effects of treatment, such as fatigue, neuropathy, and risk of secondary cancers.
- Patients are advised to report any new or ongoing symptoms to their healthcare team promptly.
Health Maintenance:
- Regular screenings for other potential health issues, such as secondary malignancies, are part of follow-up care. For example, patients who received radiation therapy may need regular mammograms or lung screenings.
- Lifestyle advice, including exercise, diet, and smoking cessation, is often provided to help maintain overall health and reduce the risk of recurrence.
Emotional and Psychosocial Support
Psychosocial Assessments:
- Emotional health is a critical component of follow-up care. Patients may receive referrals to psychologists or counselors if needed.
- Support groups and survivorship clinics can provide additional emotional and social support.
Patient Education and Self-Management:
- Patients are encouraged to take an active role in their follow-up care by monitoring their health, managing side effects, and maintaining a healthy lifestyle.
- Educational resources and support services are available to help patients navigate life after treatment.
Communication and Coordination
Coordination of Care:
- Effective communication between the cancer care team, primary care providers, and the patient is crucial for successful follow-up care.
- Patients are advised to keep detailed records of their treatment and follow-up care plans to share with all healthcare providers involved in their care.
Access to Care:
- Patients should have access to their healthcare team for any concerns between scheduled appointments. Many institutions provide contact information for patients to reach out if they have any worries about their health.
In summary, follow-up care after Burkitt lymphoma treatment is comprehensive and involves regular monitoring, managing side effects, maintaining overall health, and providing emotional support. It is tailored to the individual needs of the patient and involves coordination between various healthcare providers to ensure the best possible outcomes.
Resources
-
- American Cancer Society – Cancer.org
- Leukemia and Lymphoma Society – lls.org
- National Cancer Institute – Cancer.gov
- Epstein-Barr virus, malaria and endemic Burkitt lymphoma – PubMed
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Cancer Research Institute – cancerresearch.org
- Hyperphosphatemia and hypocalcemia in Burkitt lymphoma. Complications of chemotherapy – PubMed
- Risk factors for Burkitt lymphoma: A nested case-control study in the UK Clinical Practice Research Datalink – PubMed
- Blood Cancer UK – bloodcancer.org
- Լymphoma Research Foundation – lymphoma.org
- Wikipedia – en.wikipedia.org
