Nishant Tiwari: Educational thread on hemophagocytic lymphohistiocytosis
Nishant Tiwari, Incoming Hematology-Oncology Fellow at OU Health Stephenson Cancer Centre, shared a thread on X/Twitter:
“Educational thread on hemophagocytic lymphohistiocytosis (HLH). Not medical advice. Always open for feedback and corrections. Inspired by and studied from the recent review from The American Society of Hematology (ASH) hematology education series 2023 edition.
HLH is a life-threatening hematological emergency characterized by aberrant inflammatory response, with excessive and inappropriate T-cell activation. It poses a diagnostic challenge due to it’s overlap with many infectious and systemic diseases.
HLH-Etiology: Often triggered by:
- Infectious, autoimmune diseases
- Malignancies, immunotherapy
- Familial predisposition due to mutations in T-cell pathways
- CAR T cells, Bi-specific T-cell engager antibodies (BiTE’s)
HLH-Pathobiology: Unfettered activation of T-cells due to inadequate control of the T-Cell activation causes massive cytokine release, especially:
- IFN-gamma
- TNF-alpha
- IL-1, IL-6, IL-18
Macrophage activation causing tissue infiltration, phagocytosis and tissue destruction.
HLH-clinical features:
- Unremitting fever
- Cytopenias, especially thrombocytopenia
- Hepatosplenomegaly
- Elevated LFTs
- CNS symptoms
- Difficult to distinguish from other systemic diseases, multiple laboratory tests available to help with this distinction.
HLH-Lab Diagnosis:
- Cytopenias, deranged LFTs
- Elevated serum triglycerides
- Decreased fibrinogen
- Elevated ferritin (Typically in thousands)
- Elevated soluble CD25 levels
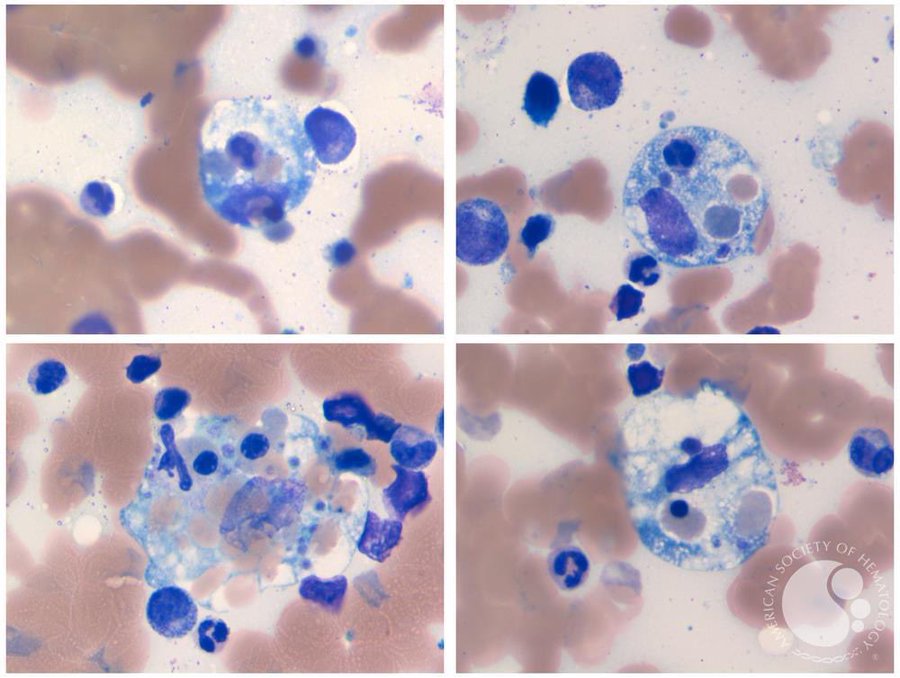
- Hemophagocytosis features on bone marrow aspirate (RBCs, WBCs in macrophage cytoplasm)
- ASH image bank image below:
HLH-Lab Diagnosis continued:
- Mutation testing for Familial-HLH
- Perforin function: STX11, STXBP2, RAB27A, LYST
- Effector T cell function: SH2D1A, ITK, CD27
- Inflammasome activation: XIAP, NLRC4
- Adult HLH is associated with somatic mutations, clonal hematopoiesis, not germline mutations
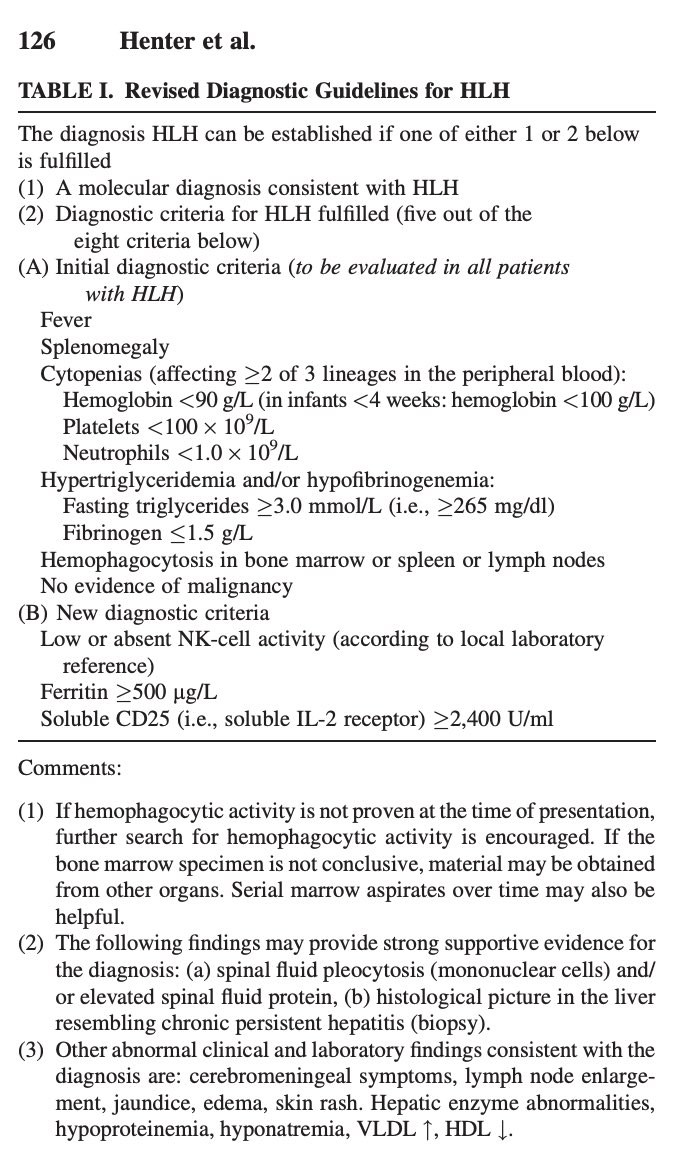
HLH diagnosis, familial HLH: HLH-2004
One of the following criteria has to be met
- Molecular diagnosis consistent with HLH
- Five of eight clinical and laboratory criteria
HLH-diagnosis, reactive-HLH, H-score: Multiple laboratory and clinical features are scored, and a score of >169 is considered a optimal diagnostic threshold for HLH.
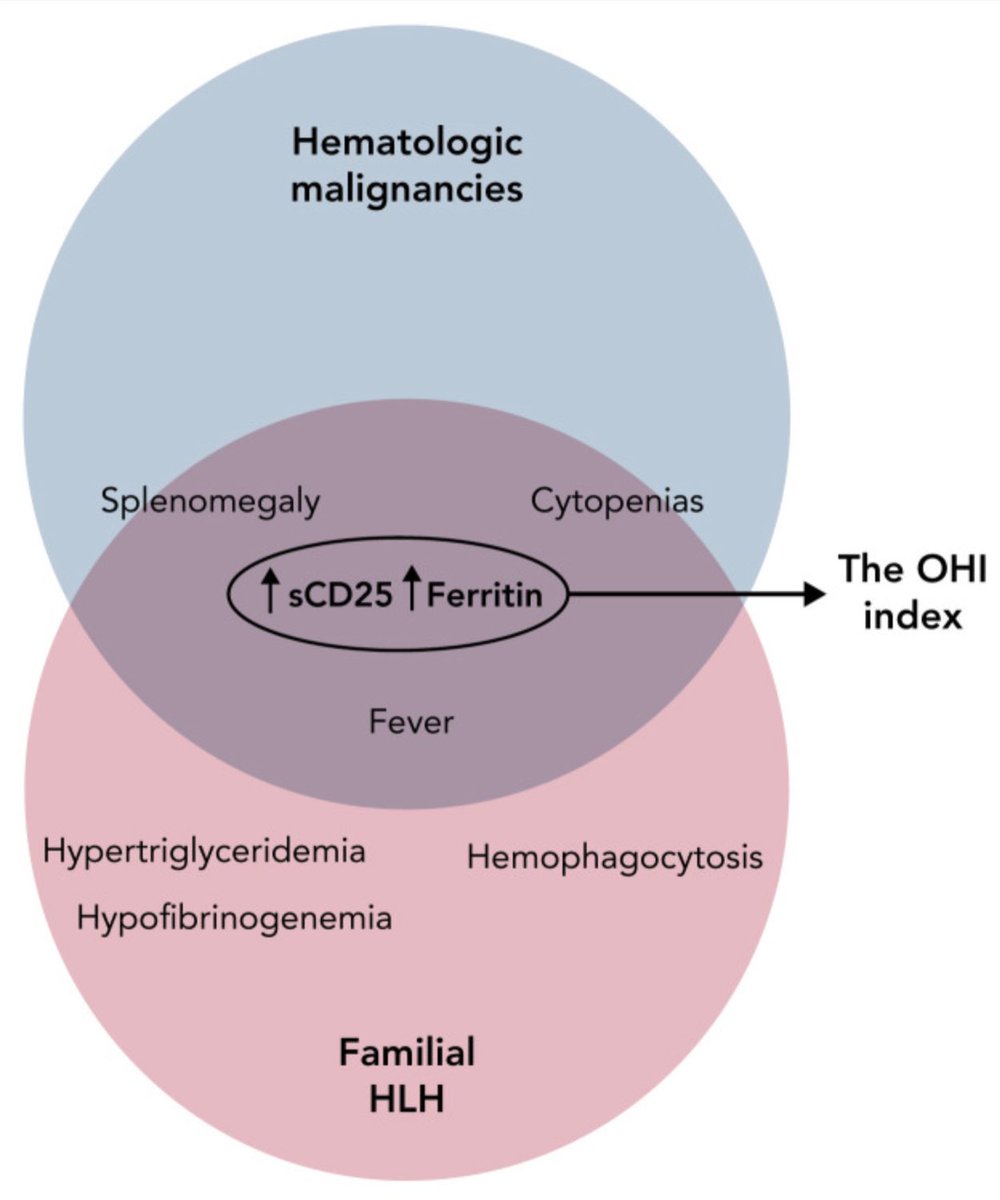
HLH-Diagnosis, Malignancy associated:
- Malignancy-associated optimized HLH inflammatory (OHI) index
- sCD25 > 3900 U/mL AND
- Ferritin > 1000 ng/mL
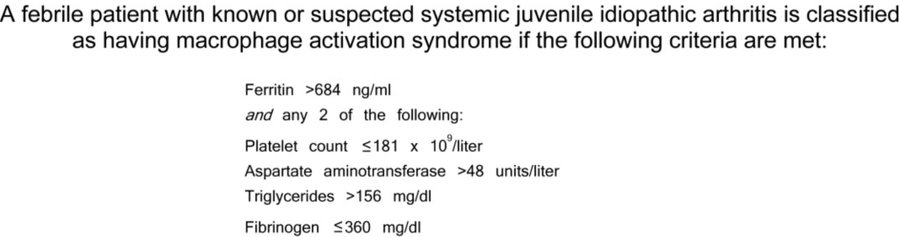
HLH diagnosis, rheumatologic 2016 EULAR/ACR criteria for macrophage activation syndrome secondary to systemic juvenile idiopathic arthritis.
Cancer and HLH:
- M-HLH: Associated with hematological malignancies, particularly lymphomas
- IC-HLH: Immune compromised (IC), occurs post chemotherapy, infectious causes
- Rx-HLH: Iatrogenic secondary to immune activation due to CAR T, BiTEs, Checkpoint inhibitors
Infections and HLH:
- Uncleared viral infections are a common triggers for familial HLH
- EBV and CMV are commonest triggers, EBV associated have poor prognosis
- COVID-19 associated cases also reported
HLH-mimics:
Conditions meeting diagnostic criteria for HLH (False +ve) -Systemic infectious states such as sepsis, disseminated TB -Atypical infections: Visceral leshmaniasis, Brucella, Ehrlichia, Bartonella, disseminated HSV, disseminated adenoviral infection, histoplasmosis.
Rheumatologic-HLH (R-HLH):
- Called macrophage activation syndrome (MAS) in the context of rheumatologic disease causing a state of hyperinflammation
- EULAR/ACR 2016 criteria used to diagnose
- IL-18 testing can differentiate between R-HLH/MAS and F-HLH
HLH-treatment:
- HLH is a medical emergency, and requires prompt treatment
- Treatment backbone is Etoposide, dexamethasone, and additional immunosuppresants
- Allo-HSCT is the standard of care for treatment of F-HLH
F-HLH-Treatment:
- Treated with HLH-94 protocol
- 8 weeks of etoposide and dexamethasone followed by Allo-HSCT -Emapalumab (Anti-IFN gamma) is used in refractory and etoposide intolerant patients
- Ongoing trials for Ruxolitinib, Tadekinig alpha (IL-18 binding protein)
M-HLH Treatment has two approaches:
- Anti-inflammatory therapy (Steroids, targeted anti-cytokine therapy, etoposide)
- Tumor specific anti-neoplastic therapy, augmented with etoposide if possible.
Rx-HLH-T/t:
- Treated with specific anticytokine therapy to retain the efficacy of immune activating therapies, such as Anakinra (Anti IL-1 receptor), Tocilizumab (Anti-IL-6 receptor)
- Data for Emapalumab (Anti-IFN-gamma) are emerging
IC-HLH-T/t:
- Diagnostic and treat the triggering/underlying infection
- Steroids and anti-cytokine as appropriate in the clinical context
R-HLH/MAS-T/t:
- Predominantly steroids are used in treatement, etoposide is rarely required
- Emapalumab, anakinra, anti-IL-6 therapies have also shown to be beneficial
HLH-T/t additional considerations:
- Infectious (PJP, anti-fungal) and stress ulcer prophylaxis should be given as appropriate
- IVIG should be given for IgG levels < 500
HLH-Dx-additional considerations:
- Early measurements of sCD25 and serum ferritin has high specificity in diagnosing HLH
- Important to remember different contexts and respective criteria used for diagnosis
Reference: (A gold standard article for better understanding).”
Source: Nishant Tiwari/X