Acute Lymphoblastic Leukemia (ALL) in children: What patients and caregivers should know about
Acute lymphoblastic leukemia (ALL) is the most common type of cancer in children, accounting for about 25% of all cancers in those under the age of 15, and is particularly prevalent among children aged 2 to 5 years 1,2. In the United States, ALL represents 20% of all cancers diagnosed in persons aged under 20 years, translating to more than 3,000 new cases annually.
This comprehensive guide aims to provide patients and caregivers with essential information about the symptoms, causes, diagnosis, treatment, prognosis, and ongoing clinical trials for ALL. Additionally, it offers practical advice on what patients should do following a diagnosis.
What is Acute lymphoblastic leukemia?
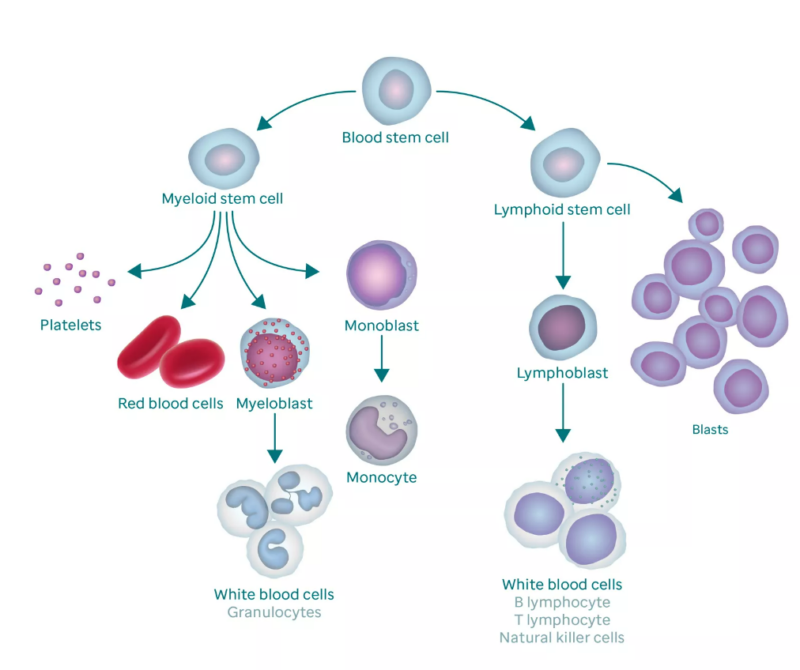
Acute lymphoblastic leukemia affects white blood cells called lymphocytes. Image from St. Jude
Acute Lymphoblastic Leukemia (ALL) is a type of cancer that originates from the early versions of white blood cells known as lymphocytes in the bone marrow. It affects both children and adults, though it is most commonly diagnosed in younger individuals. The disease is characterized by the malignant transformation and proliferation of lymphoid progenitor cells, which can spread to the blood and other parts of the body3,4.
Types of ALL
ALL can arise from different types of lymphocytes, leading to various forms of the disease. The two main types of lymphocytes involved are:
- B-lymphocytes (B-cells): Most cases of ALL are of B-cell origin. This form is called B-ALL or pre-B ALL5.
- T-lymphocytes (T-cells): A smaller percentage of cases arise from T-cells, known as T-ALL5.
These lymphocytes are crucial components of the immune system, responsible for detecting and eliminating pathogens like bacteria and viruses. However, in ALL, these cells are produced in an immature form called lymphoblasts, which are ineffective at fighting infections and multiply uncontrollably8.
Prevalence and Demographics
Ethnicity and Race
- Hispanic Populations: Hispanic children have the highest incidence rates of ALL, with studies showing a rate of 42.9 cases per million6. They are reported to have a 30-40% higher risk compared to non-Hispanic populations 7.
- Non-Hispanic Whites: This group also shows a significant number of ALL cases, though less than Hispanics 8.
- Non-Hispanic Blacks and Other Races: The incidence among non-Hispanic blacks ranges from 10.1 to 27.9 per 1 million, which is lower compared to Hispanics and non-Hispanic whites 6. Asian and African American children have lower rates of ALL compared to Hispanic and White children 8.
Age and gender
- The peak incidence of ALL occurs in children aged 2-5 years 3,8. This age group is particularly vulnerable, although ALL can occur at any age during childhood and adolescence.
- ALL is more common in boys than in girls. The reasons for this difference are not fully understood but have been consistently observed across various studies 8.
Geographic Variations
- In the United States, the incidence of pediatric ALL was highest in the West U.S. Census Region, a trend possibly reflecting the higher proportion of Hispanics in many of the region’s states 6.
- Specific states like California, New Mexico, and Vermont have been identified with the highest rates of pediatric ALL incidence6.
Symptoms of Acute Lymphoblastic Leukemia
The early symptoms of ALL can be quite general and often mimic those of other common childhood illnesses. However, recognizing these signs early can lead to timely diagnosis and treatment, which significantly improves the prognosis. Common symptoms include 9,10,11,.
- Fever and Infections: Many children with ALL experience fevers that are not related to a specific infection. Due to the leukemia affecting the immune system, children may also have frequent or severe infections12,13.
- Bruising and Bleeding: Children with ALL may show unusual bruising or bleeding due to low platelet counts. This can include frequent nosebleeds, bleeding gums, and petechiae (tiny red spots on the skin)13.
- Bone and Joint Pain: Pain in bones and joints is a common symptom, often caused by the overcrowding of bone marrow with abnormal cells. This can lead to children experiencing limping or reluctance to engage in usual activities 13.
- Anemia: Due to the high number of leukemia cells in the bone marrow, there is often a reduced production of normal red blood cells, leading to anemia. Symptoms of anemia include fatigue, pallor, and breathlessness6.
- Abdominal Pain and Swelling: The liver and spleen may become enlarged due to the accumulation of leukemia cells, causing pain or a feeling of fullness in the abdomen13.
- Swollen Lymph Nodes: Lymph nodes in the neck, armpits, stomach, or groin may become swollen due to the accumulation of leukemia cells13.
- Difficulty Breathing: In some cases, leukemia cells can form a mass in the chest, for example, acute T lymphoblastic leukemia sometimes can be associated with Thymoma leading to pain and difficulty breathing 14.
- Other Symptoms: Additional symptoms can include severe or persistent headaches, vomiting, blurred vision, or unexplained weight loss, which may indicate the spread of leukemia cells to other parts of the body like the central nervous system6,13.
These symptoms are not exclusive to ALL and can be indicative of other health issues, so they must be evaluated by a healthcare provider for an accurate diagnosis 6,13.
A short video about Acute Lymphoblastic Leukemia from “Medical Centric”
Causes and Risk Factors
While the exact cause of ALL is not fully understood, several risk factors have been identified17.
- Genetic predisposition: Certain genetic disorders like Down syndrome are linked to an increased risk of developing ALL.
- Environmental exposures: Previous cancer treatments, such as chemotherapy and radiation, or exposure to high levels of radiation can increase the risk.
- Random genetic mutations: Most cases of ALL as in other cancers result from mutations that occur randomly and are not inherited from parents.
Diagnosis of Acute Lymphoblastic Leukemia
Diagnosing ALL typically involves a series of tests 5,13.
- Blood tests: These can show abnormal levels of white blood cells and low levels of platelets and red blood cells.
- Bone marrow biopsy: A sample of bone marrow is taken, usually from the hip, to look for the presence of leukemia cells.
- Imaging tests: X-rays, MRI, or CT scans may be used to check for swollen lymph nodes or other organs affected by the spread of leukemia cells.
- Lumbar puncture (spinal tap): This test checks for leukemia cells in the fluid around the brain and spinal cord.
Watch a nice video about Bone Marrow Biopsy by “Learn from Lincoln”.
Treatment Options
Treatment for ALL is typically aggressive and can last for two to three years. The following are the main treatment options used today. The selection of the specific treatment type depends on the cancer subtype, disease stage, and patient’s responsiveness to treatment.
Chemotherapy
- Main Treatment: Chemotherapy is the cornerstone of ALL treatment, involving drugs that kill cancer cells. It’s divided into three phases: induction, consolidation, and maintenance 6,17.
- Intrathecal medications/chemotherapy. Intrathecal chemotherapy is chemotherapy that is injected into the spinal fluid to prevent or treat leukemia in the brain and spinal cord. Intrathecal medications/chemotherapy involves inserting medications through a needle into the fluid-filled space surrounding the spinal cord.
Radiation Therapy
- Targeted Radiation: Uses high-energy rays to kill cancer cells, sometimes used to treat or prevent the spread of leukemia to the brain and spinal cord 17.
Stem Cell Transplantation
- Bone Marrow Transplant: Replaces diseased bone marrow with healthy marrow from a donor, used in high-risk cases or when chemotherapy is not effective 17. Blood and marrow transplantation consists of three steps:
1) collection of healthy stem cells from a donor without cancer or from the patient himself or herself
2) administration of high doses of chemotherapy and possibly radiation therapy to kill any remaining leukemia cells
3) infusion of the healthy stem cells through an intravenous line to produce normal blood-forming cells.
Bone marrow or stem cell transplantation is commonly used to treat ALL that has not responded to chemotherapy, or that was found to have a very high risk of relapse.
Targeted Therapy
- Precision Medicine: Involves drugs that specifically target abnormalities in cancer cells. For example, drugs like imatinib are used for Philadelphia chromosome-positive ALL 6.
Immunotherapy
- CAR-T Cell Therapy: A treatment where a patient’s T cells are genetically engineered to better recognize and attack leukemia cells 18.
- Monoclonal Antibodies: Drugs that help the immune system find and destroy cancer cells, such as blinatumomab 6.
Treatment of recurrent ALL
For children with relapsed Acute Lymphoblastic Leukemia (ALL), the treatment approach is highly dependent on the timing of the relapse post-initial treatment. If leukemia returns after a significant period, the initial chemotherapy regimen might still be effective, and similar drugs could be used to achieve a second remission.
This treatment might include chemotherapy drugs such as vincristine, L-asparaginase, anthracyclines (like doxorubicin, daunorubicin, or mitoxantrone), cyclophosphamide, cytarabine (ara-C), and either etoposide or teniposide, along with a steroid (prednisone or dexamethasone).
Intrathecal chemotherapy is also administered to target leukemia cells in the cerebrospinal fluid (CSF)17,18. In cases where ALL recurs shortly after the initial treatment or in children with T-cell ALL who experience a relapse, the treatment strategy might be more aggressive, potentially including a stem cell transplant, especially if there is a sibling match for the tissue type. This approach is also considered for children who relapse after a second chemotherapy course17,18.
For extramedullary relapse, where leukemia cells are found in specific body parts like the CSF or testicles but not in the bone marrow, the treatment includes intensive chemotherapy along with more intense intrathecal chemotherapy. If the relapse occurs in the brain and spinal cord areas not previously treated with radiation, radiation therapy might be added. Boys experiencing a relapse in a testicle may receive radiation to that area17,18.
If ALL does not respond to treatment or recurs post-stem cell transplant, newer immunotherapy options may be considered. These include CAR T-cell therapy, which involves modifying the patient’s T cells to target leukemia cells, and blinatumomab (Blincyto), a bispecific T cell engager that brings T cells and cancer cells together to enhance the immune system’s ability to kill cancer cells. Another option is inotuzumab ozogamicin (Besponsa), an antibody-drug conjugate that targets CD22, a protein found on the surface of ALL cells, delivering a cytotoxic agent directly to them17,18.
Watch the Avalynn’s Battle with Childhood Leukemia from “Johns Hopkins All Children’s Hospital”
Ongoing clinical trials and newest treatment options
These novel therapies and clinical trials represent significant advancements in the treatment of pediatric ALL, offering hope for improved outcomes and reduced side effects compared to traditional chemotherapy regimens.
The ongoing research and development in this field continue to push the boundaries of what is possible in oncology, aiming for higher survival rates and better quality of life for affected children 18,19,20
- CAR T-Cell Therapy: Several sources highlight the efficacy of CAR T-cell therapy in pediatric ALL. For instance, tisagenlecleucel (Kymriah®) has shown promising results in children and young adults with relapsed or refractory B-cell ALL, achieving sustained remissions 8,21. This therapy involves modifying the patient’s own T-cells to target and kill leukemia cells.
- Blinatumomab: This is a bispecific T-cell engager (BiTE) antibody that brings T-cells into close contact with B-cells, leading to the destruction of the leukemia cells. Clinical trials have shown that blinatumomab is effective in treating pediatric patients with relapsed or refractory ALL, offering a significant therapeutic option17,18.
- Nelarabine: Approved for use in relapsed T-cell ALL, nelarabine has been shown to be effective as a single agent, particularly in pediatric patients17. It is a chemotherapy drug that is specifically toxic to T-cells and is used in cases where other treatments have failed.
- Inotuzumab Ozogamicin: This is an antibody-drug conjugate that targets CD22, a protein expressed on the surface of B-cells. It has been used in clinical trials for pediatric ALL and has shown efficacy, particularly in patients with relapsed or refractory disease20.
- Tyrosine Kinase Inhibitors (TKIs): For patients with Philadelphia chromosome-positive (Ph+) ALL, TKIs such as imatinib have been used successfully. These drugs block the function of the BCR-ABL fusion protein that drives the growth of leukemia cells21.
- Venetoclax: This drug targets the BCL-2 protein, which helps cancer cells survive. It is being studied in combination with chemotherapy and has shown potential in various clinical trials for enhancing the treatment of pediatric ALL17.
- Daratumumab: This monoclonal antibody targets CD38 and has been explored in pediatric patients with ALL. It has shown promise in early clinical trials, particularly for patients who have relapsed or are refractory to other treatments18.
Minimal Residual Disease (MRD) Monitoring and Treatment: Clinical trials are increasingly using MRD as a measure to tailor therapy intensity. If standard lab tests show the leukemia seems to have gone away, more sensitive tests may be used to look for even small numbers of remaining leukemia cells (known as minimal residual disease, or MRD).
MRD-negative status is associated with a better prognosis, and treatments may be intensified or de-escalated based on MRD results to optimize outcomes and minimize toxicity21. If the leukemia remains despite chemotherapy, newer types of immunotherapy such as CAR T-cell therapy or blinatumomab (Blincyto), or the antibody-drug conjugate inotuzumab ozogamicin (Besponsa) might be options.
Prognosis
The prognosis for children with ALL has improved significantly over the past few decades, with current survival rates around 90%22. Factors affecting prognosis include the patient’s age at diagnosis, initial white blood cell count, and response to initial treatment23,24.
Watch the survival story of Elaina
Patient’s Survivorship
Treatment for pediatric ALL has improved dramatically over the past half-century, leading to high survival rates. However, both during and after treatment, patients may face a range of problems or side effects, which require careful management and follow-up.
Problems During Treatment
1. Infections: Due to the immunosuppressive effects of chemotherapy, children with ALL are at increased risk of infections. Effective management includes aggressive immunosuppression, with corticosteroids being the cornerstone of treatment. However, over half of the patients may experience severe infections during treatment25.
2. Anemia and Bleeding: Chemotherapy can lead to reduced production of red blood cells (causing anemia) and platelets (increasing the risk of bleeding). Treatment may include blood transfusions and medications to stimulate blood cell production.
3. Nausea and Vomiting: These are common side effects of chemotherapy and can be managed with anti-nausea medications26.
4. Fatigue: Fatigue is a pervasive issue during ALL treatment, often resulting from anemia, the leukemia itself, or as a side effect of chemotherapy26.
Problems After Treatment
1. Secondary Malignant Neoplasms (SMNs): There is a small risk of developing acute myeloid leukemia (AML) or other cancers as a result of chemotherapy drugs such as epipodophyllotoxins, alkylating agents, or anthracyclines27.
2. Cardiac Dysfunction: Certain chemotherapy drugs or radiation therapy to the chest can sometimes cause heart or lung problems later in life27.
3. Learning Problems: Treatment that includes radiation therapy to the brain or some types of chemotherapy may affect learning ability in some children27.
4. Growth and Development Issues: Some cancer treatments may affect a child’s growth, leading to short stature or affecting hormone levels, which can increase the risk of health issues such as thyroid problems, obesity, and diabetes27.
5. Fertility Issues: Cancer treatment may also affect sexual development and the ability to have children later in life27.
6. Bone Problems: Bone damage or osteoporosis may result from the use of prednisone, dexamethasone, or other steroid drugs27.
What Patients Should Do
1. Regular Follow-Up: Survivors of pediatric ALL must have regular follow-up appointments to monitor for late effects of treatment and manage any that arise. This includes screenings for heart health, growth and development assessments, and fertility evaluations26,27.
2. Healthy Lifestyle: Adopting a healthy lifestyle, including a balanced diet and regular physical activity, can help mitigate some long-term effects of treatment26.
3. Psychological Support: Psychological support for the child and family is important to address any emotional or mental health issues that may arise during or after treatment26.
4. Education Plan: For children who experience learning difficulties, an individualized education plan (IEP) may be necessary to address their specific needs27.
5. Discuss Fertility Preservation: Before treatment begins, discuss fertility preservation options with the healthcare team. This may include sperm banking or other methods depending on the age and development of the child27.
In summary, while the treatment of pediatric ALL has seen significant advancements, attention to the potential side effects during and after treatment is essential for the overall well-being of the child.
A multidisciplinary approach involving oncologists, pediatricians, endocrinologists, psychologists, and other specialists is key to managing these challenges effectively.
This video shows the patient’s treatment in the first 30 days in “POGO (Pediatric Oncology Group of Ontario)”
Conclusion
Acute lymphoblastic leukemia in children is a serious but increasingly treatable disease. Advances in treatment have significantly improved outcomes, making early diagnosis and adherence to treatment plans critical.
Ongoing research and clinical trials continue to push the boundaries of what is possible in ALL treatments, offering hope for even better survival rates and quality of life in the future.
References and useful resources
St. Jude Children’s Research Hospital – The Together by St. Jude™ online resource provides trusted information about childhood and adolescent cancer, blood disorders, and other life-threatening diseases.
Clinicaltrials.gov – a huge database of clinical trials, useful for patients and families to find past, ongoing, and upcoming clinical trials.
Cancer.Net – Comprehensive information for people with cancer, families, and caregivers, from the American Society of Clinical Oncology (ASCO)
Cancer.Gov – More comprehensive overview on the treatment of childhood acute lymphoblastic leukemia by NCI
Chop.edu – Children’s Hospital of Philadelphia
Cancer.org – American Cancer Society
Leukemia and Lymphoma Society – national, voluntary health agency dedicated to curing leukemia, lymphoma, Hodgkin’s disease, and myeloma, and to improving the quality of life of patients and their families.
Oncodaily.com – Online platform where you can find anything related to cancer such as everyday news, blogs, videos, podcasts, etc.