Immunotherapy use and effectiveness in Child-Pugh class B
JAMA Oncology shared a post on X about a paper titled “Immunotherapy vs Best Supportive Care for Patients With Hepatocellular Cancer With Child-Pugh B Dysfunction” published in JAMA Network.
Authors:

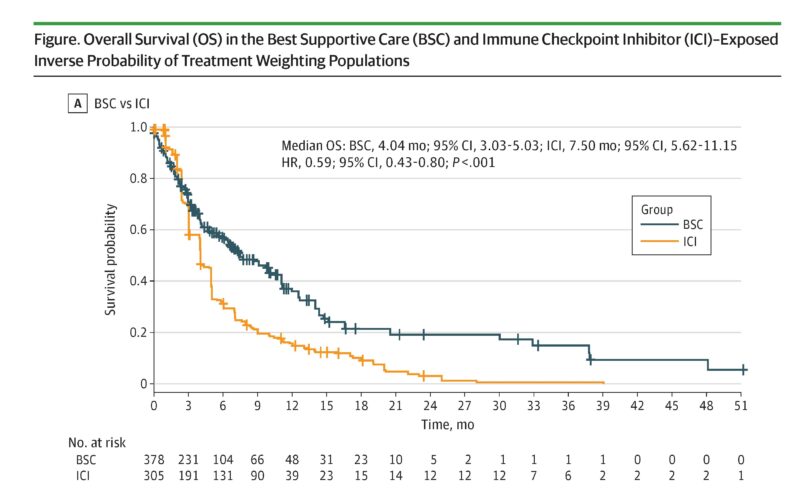
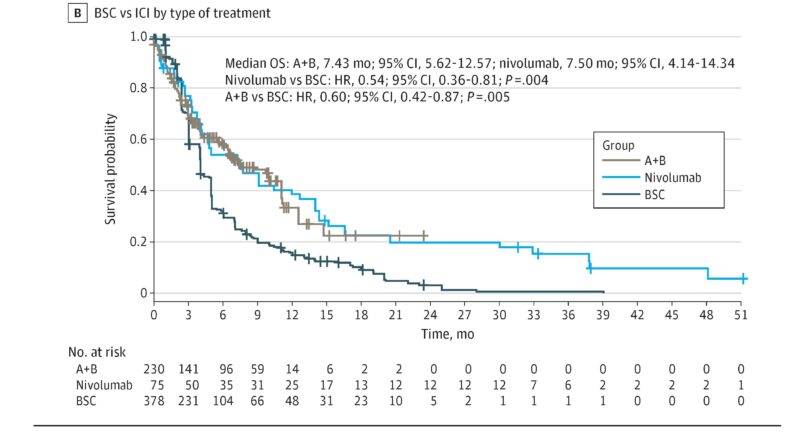
“In this case series of patients with Child-Pugh class B liver dysfunction, immunotherapy-based systemic therapy was associated with reduction in the risk of death compared with best supportive care.”
Nina Niu Sanford shared the post by JAMA Oncology, adding:
“To me it is remarkable that median OS in Child Pugh B with ICI is only 7.5 months.
Liver disease major competing risk, plus advanced liver dysfunction likely causes immunosuppression/reduced responsiveness to ICI.
Can’t imagine ICI being cost-effective in this group.
Also, the 7.5 months here likely inflated due to selection bias and ~90% of patients being B7/8 (would guess mostly 7) – larger study showed OS for Child Pugh B was 5.5 months, much lower than Child Pugh A, and hardly better than BSC.”
Enrique Soto also shared comments about the paper:
“Not surprisingly, patients we were in significantly worse shape had worse outcomes (slightly) than those who were better off… Absolutely useless information for clinical care, and probably hurtful for patients.”
Source: JAMA Oncology/X, Nina Niu Sanford/X and Enrique Soto/X
Dr. Nina Niu Sanford is an Assistant Professor and Chief of Gastrointestinal Radiation Oncology at Harvard/Brigham and Women’s Hospital/Massachusetts General Hospital. She specializes in treating gastrointestinal cancers and actively participates in clinical trials combining high-dose radiation therapy with immunotherapy. Additionally, she researches healthcare access disparities and conducts pan-cancer outcomes research using large databases.
Dr. Soto Pérez de Celis is a geriatric oncologist and researcher in the Department of Geriatrics at the Salvador Zubirán National Institute of Health Sciences and Nutrition in Mexico City. He serves as a liaison to the ASCO Evidence-Based Medicine Committee and is a member of the Society’s Finance Committee. His research focuses on using mobile technology to monitor older adults with cancer undergoing chemotherapy and addressing global disparities in cancer care.
