
Vaginal Cancer: What patients should know about
Introduction
Vaginal cancer is a rare type of cancer that begins in the vagina. It accounts for only 1-2% of all gynecological cancers. Understanding the causes, risk factors, symptoms, and treatment options is crucial for patients diagnosed with or at risk of vaginal cancer. This article aims to provide comprehensive, patient-friendly information on vaginal cancer.
Causes, Risk Factors, and Subtypes
Causes
The exact cause of vaginal cancer is not fully understood. However, it is known that certain factors can increase the risk of developing this cancer. Vaginal cancer occurs when healthy cells in the vagina undergo changes in their DNA, leading to uncontrolled growth and the formation of a tumor.
Risk Factors
- Age: The risk of vaginal cancer increases with age, with most cases diagnosed in women over 60.
- Human Papillomavirus (HPV): HPV infection is a significant risk factor. HPV types 16 and 18 are most strongly linked to vaginal cancer.
- Diethylstilbestrol (DES): Diethylstilbestrol (DES) is a synthetic nonsteroidal estrogen, which was widely prescribed to pregnant women between 1938 and 1971 to prevent miscarriages and other pregnancy complications, such as premature delivery. Women whose mothers took DES during pregnancy are at higher risk of developing clear cell adenocarcinoma, a subtype of vaginal cancer.
- Smoking: Smoking doubles the risk of vaginal cancer.
- Previous Cancer: A history of cervical cancer or precancerous conditions can increase the risk.
- Weakened Immune System: Conditions like HIV/AIDS or medications that suppress the immune system can increase the risk.
- Vaginal Adenosis: This condition, where glandular cells line the vagina instead of squamous cells, can increase the risk.
Subtypes
- Squamous Cell Carcinoma: The most common type, accounting for about 90% of vaginal cancers. It develops in the squamous cells lining the vagina.
- Adenocarcinoma: Originates in the glandular cells of the vagina and accounts for about 5-10% of cases.
- Clear Cell Adenocarcinoma: Linked to DES exposure in utero.
- Melanoma: A rare type that begins in the pigment-producing cells.
- Sarcoma: Develops in the deeper tissues of the vagina and includes types like rhabdomyosarcoma and leiomyosarcoma.
Vaginal Cancer Symptoms
Vaginal cancer may not cause symptoms in its early stages. As the cancer grows, symptoms may include:
- Abnormal Vaginal Bleeding: This can occur after intercourse, between periods, or after menopause. It happens because the tumor disrupts the normal blood vessels in the vaginal lining.
- Vaginal Discharge: This may be watery, blood-stained, or have a foul odor due to the presence of cancer cells and infection.
- Lump or Mass in the Vagina: A palpable mass may be felt, indicating the presence of a tumor.
- Pain During Intercourse: The tumor can cause discomfort or pain during sexual activity.
- Painful Urination: This occurs if the tumor presses on the bladder or urethra.
- Constipation: If the tumor presses on the rectum, it can cause difficulty in bowel movements.
- Pelvic Pain: Pain in the lower abdomen or pelvis can occur as the cancer spreads to nearby tissues.
- Back Pain and Leg Swelling: Advanced cancer can cause these symptoms due to the spread to lymph nodes and other structures.
Diagnosis
Diagnosing vaginal cancer involves several steps:
- Physical Examination: A thorough pelvic exam may be performed to check for abnormalities.
- Pap Test: This screening test can help to detect precancerous or cancerous cells in the cervix and vagina.
- Colposcopy: A procedure using a special magnifying device to examine the vagina and cervix more closely.
- Biopsy: A sample of tissue is taken from the suspicious area and examined under a microscope to confirm the presence of cancer cells.
- Imaging Tests: Tests like MRI, CT scans, and PET scans may be used to determine the extent of the cancer and whether it has spread.
Prevention
While it is not always possible to prevent vaginal cancer, certain measures can reduce the risk:
- HPV Vaccination: Vaccines can protect against the types of HPV most commonly linked to cancer.
- Regular Screening: Routine pelvic exams and Pap tests can help detect precancerous changes early.
- Quit Smoking: Stopping smoking can reduce the risk of many cancers, including vaginal cancer.
- Safe Sexual Practices: Using condoms and limiting the number of sexual partners can reduce the risk of HPV infection.
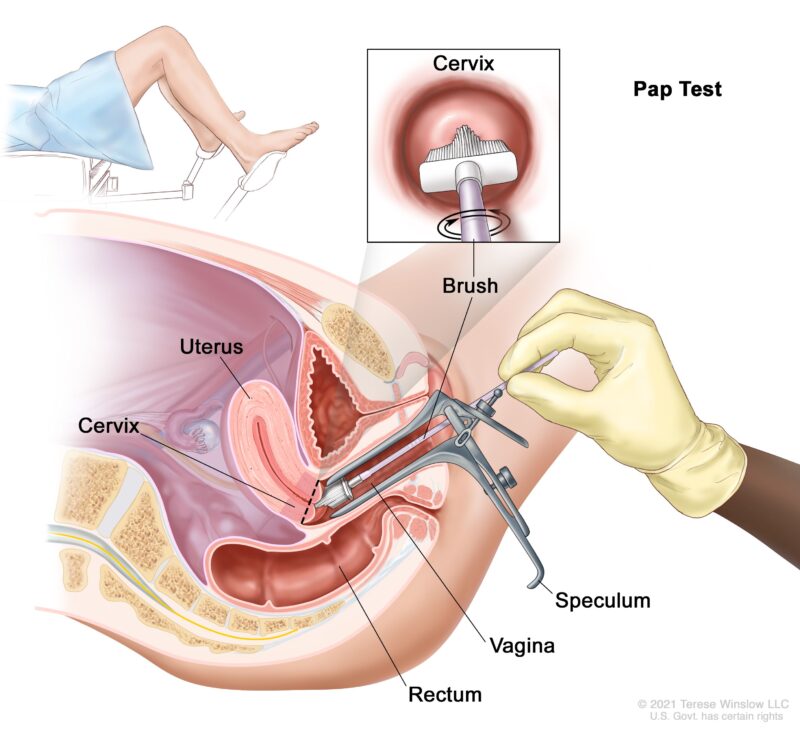
This image is taken from cancer.gov
Prognosis
The prognosis for vaginal cancer depends on several factors, including the stage at diagnosis, the type of cancer, and the patient’s overall health. Early-stage vaginal cancer has a better prognosis and is more likely to be treated successfully. Advanced-stage cancer, which has spread beyond the vagina, is more challenging to treat and has a lower survival rate.
Treatment and Side Effects
Understanding the treatment options for vaginal cancer and their potential side effects can help patients make informed decisions about their care. Selection of one or another treatment option usually depends on the stage of disease as well as the patient’s overall health and associated conditions. Here is a detailed overview of the common treatments and their side effects.
Surgery
Surgery is often used to remove the tumor and some surrounding tissue.
Types of Surgery
- Local Excision: This involves removing the tumor and a small margin of healthy tissue around it. It is often used for early-stage cancers.
- Partial Vaginectomy: This procedure removes part of the vagina and is used when the cancer is confined to a specific area.
- Total Vaginectomy: This involves removing the entire vagina and is used for more extensive cancers.
- Radical Vaginectomy: This surgery removes the vagina and surrounding tissues and is used for advanced cancers.
- Lymph Node Dissection: This involves removing lymph nodes in the pelvis or groin to check for cancer spread.
- Reconstructive Surgery: After a vaginectomy, reconstructive surgery may be performed to create a new vagina using skin and muscle from other parts of the body.
Side Effects of Surgery
- Pain: Pain is common after surgery and can be managed with pain medications.
- Infection: There is a risk of infection at the surgical site, which can be managed with antibiotics.
- Changes in Sexual Function: Surgery can affect sexual function and sensation. Reconstructive surgery can help, and counseling may be beneficial.
- Difficulty Urinating: There may be temporary or permanent changes in urination patterns.
- Lymphoedema: Swelling in the legs can occur if lymph nodes are removed.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It can be delivered externally or internally (brachytherapy).
Types of Radiation Therapy
- External Beam Radiation Therapy (EBRT): Radiation is directed at the cancer from a machine outside the body. This is often used for larger tumors or when cancer has spread to nearby lymph nodes.
- Internal Radiation Therapy (Brachytherapy): Radioactive material is placed inside the vagina near the cancer. This is often used for smaller, localized tumors.
Side Effects of Radiation Therapy
- Skin Irritation: The treated area may become red, dry, and peel, similar to a sunburn.
- Fatigue: Feeling tired is common during and after treatment.
- Vaginal Dryness and Stenosis: The vagina may become dry, shorter, and narrower, making intercourse painful. Using vaginal dilators and lubricants can help.
- Bladder and Bowel Changes: There may be an increased frequency of urination, a burning sensation, diarrhea, and abdominal cramps.
- Early Menopause: If the ovaries are affected, leading to symptoms like hot flashes and vaginal dryness.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It is often used in combination with radiation therapy, especially for advanced cancers.
Side Effects of Chemotherapy
- Nausea and Vomiting: These can be managed with anti-nausea medications.
- Hair Loss: Hair loss is temporary and usually grows back after treatment.
- Fatigue: Feeling tired is common and can be managed with rest and light exercise.
- Increased Risk of Infection: This is due to low white blood cell counts.
- Mouth Sores: Painful sores can develop in the mouth and throat.
- Loss of Appetite: This can lead to weight loss.
- Diarrhea or Constipation: These can be managed with dietary changes and medications.
- Premature Menopause: This can lead to symptoms like hot flashes and vaginal dryness.
Targeted Therapy
Targeted therapy uses drugs that specifically target molecules involved in cancer growth. This treatment is less common for vaginal cancer but may be used in certain cases.
FDA-Approved Agents for Vaginal Cancer
- Bevacizumab: Bevacizumab is an angiogenesis inhibitor that targets the vascular endothelial growth factor (VEGF). It is used to treat advanced vaginal cancer, particularly when it has spread or recurred. Bevacizumab works by inhibiting the formation of new blood vessels that tumors need to grow and spread. It is often used in combination with chemotherapy.
- Pembrolizumab: Pembrolizumab is an immune checkpoint inhibitor that targets the PD-1/PD-L1 pathway. It is used for treating various cancers, including vaginal cancer, especially in cases where the cancer expresses PD-L1. Pembrolizumab helps the immune system recognize and attack cancer cells more effectively.
Side Effects of Targeted Therapy
- Skin Rash: This is common with some targeted therapies.
- Diarrhea: This can be managed with medications and dietary changes.
- Fatigue: This can be managed with rest and light exercise.
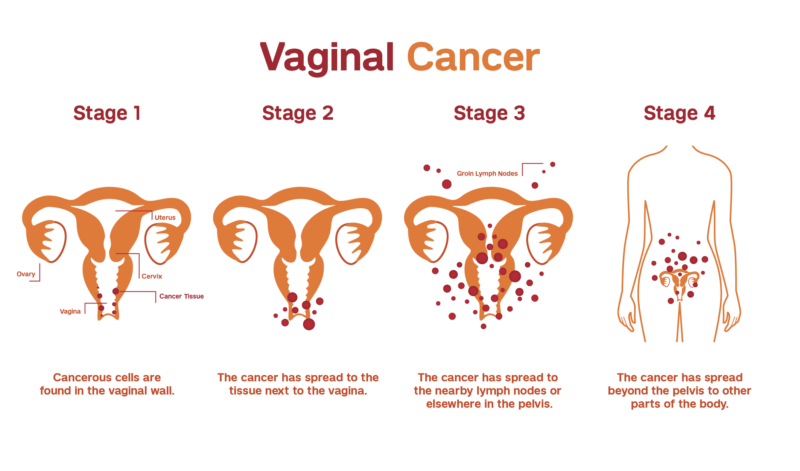
This image is taken from weillcornell.org
Newest Options and Ongoing Trials
Research is ongoing to find new and more effective treatments for vaginal cancer. Clinical trials are testing new drugs, combinations of treatments, and innovative approaches like immunotherapy. Patients may consider participating in clinical trials to access cutting-edge treatments and contribute to medical research.
More information about ongoing clinical trials can be found on clinicaltirals.gov
Patient Survivorship
Impact of Vaginal Cancer on Sexual Health
Vaginal cancer and its treatments can lead to several sexual health issues. These issues can arise from the physical changes caused by the cancer itself, as well as the side effects of treatments such as surgery, radiation therapy, and chemotherapy.
Physical Changes
- Vaginal Dryness and Atrophy: Treatments like radiation therapy can cause the vaginal tissues to become thin, dry, and less elastic. This condition, known as vaginal atrophy, can make intercourse painful.
- Vaginal Stenosis: Radiation therapy can lead to the narrowing and shortening of the vagina, a condition called vaginal stenosis. This can make penetration during intercourse difficult and painful.
- Scarring and Fibrosis: Surgery and radiation can cause scarring and fibrosis (thickening and hardening of tissues), which can affect the flexibility and function of the vagina.
- Changes in Sensation: Surgery, especially if it involves nerve damage, can alter sensation in the genital area, leading to changes in sexual pleasure and response.
Hormonal Changes
- Early Menopause: Treatments that involve the removal of the ovaries or damage to the ovaries from radiation can lead to early menopause. This results in a sudden drop in estrogen levels, causing symptoms like hot flashes, night sweats, vaginal dryness, and decreased libido.
- Hormonal Imbalance: Chemotherapy and other treatments can disrupt the balance of hormones, leading to reduced levels of estrogen, progesterone, and testosterone, which are important for sexual health and function.
Psychological and Emotional Impact
- Body Image Concerns: Changes in the appearance of the genital area due to surgery or radiation can affect a woman’s body image and self-esteem. This can lead to feelings of embarrassment and reluctance to engage in sexual activity.
- Anxiety and Depression: The diagnosis of cancer and the stress of treatment can lead to anxiety and depression, which can further reduce sexual desire and enjoyment.
- Relationship Strain: Changes in sexual function and desire can strain relationships. Open communication with partners and seeking counseling can help manage these challenges.
This video is taken from Stand Up To Cancer UK
Conclusion
Vaginal cancer is a rare but serious condition that requires prompt diagnosis and treatment. Understanding the risk factors, symptoms, and treatment options can help patients make informed decisions about their care. Regular screening and preventive measures can reduce the risk of developing vaginal cancer. Survivors may face ongoing challenges, but with the right support and care, they can manage these difficulties and maintain a good quality of life.
References
- Risk Factors for Vaginal Cancer – cancer.org
- Vaginal Cancer Causes & Factors That Put You at Risk – cancercenter.com
- Symptoms of Vaginal Cancer – NHS.uh
- Risks and Causes of Vaginal Cancer – cancerresearchuk.org
- Vaginal Cancer: Symptoms and Signs – cancer.net
- A Qualitative Study of Sexual Health and Function of Females with Pelvic Cancer
- Maintaining Sexual Health Throughout Gynecologic Cancer
- A Comprehensive Discussion in Vaginal Cancer Based on Current Research
- Vaginal Cancer – StatPearls – NCBI Bookshelf
- Women, Sexual Health, and Cancer | OncoLink.org
- Sexual Health Issues in Women and Cancer Treatment – Side Effects – cancer.gov
- Vaginal Cancer: Introduction – cancer.net
