Glioblastoma in Adults: What patients should know about
Glioblastoma, also known as glioblastoma multiforme, is the most aggressive and common type of primary brain cancer. It originates from astrocytes, the star-shaped cells that support nerve cells, and can occur in the brain or spinal cord. These tumors are highly malignant, characterized by rapid growth and the ability to invade and destroy healthy brain tissue. They are classified as grade IV tumors by the World Health Organization (WHO) due to their high level of malignancy and poor prognosis. Symptoms often include headaches, nausea, seizures, and cognitive impairments, which can progress rapidly. Despite significant advances in medical research and treatment strategies, this tumor remains a challenge, with a poor prognosis and limited treatment options.
Prevalence and Epidemiology
Glioblastoma is a relatively rare cancer, with an estimated annual incidence rate of approximately 3.2 cases per 100,000 individuals in the United States. However, it accounts for a significant portion of all primary brain tumors, making it a significant public health concern.
The incidence of this tumor varies across different age groups, with a higher prevalence among older adults. The median age at diagnosis is 64 years, and the risk increases with age, peaking around the seventh decade of life. Glioblastoma is slightly more common in men than in women, with a male-to-female ratio of approximately 1.6:1.
Types
Glioblastoma is classified into two main types based on its molecular characteristics and clinical presentation:
- Primary (de novo) glioblastoma: This type accounts for approximately 90% of all glioblastoma cases and typically develops rapidly, with no evidence of a less malignant precursor lesion. Primary glioblastomas are more common in older adults and are associated with a poorer prognosis.
- Secondary glioblastoma: This type develops from a lower-grade astrocytoma (a type of glioma) that has progressed over time. Secondary glioblastomas are more common in younger patients and tend to have a slightly better prognosis compared to primary glioblastomas.
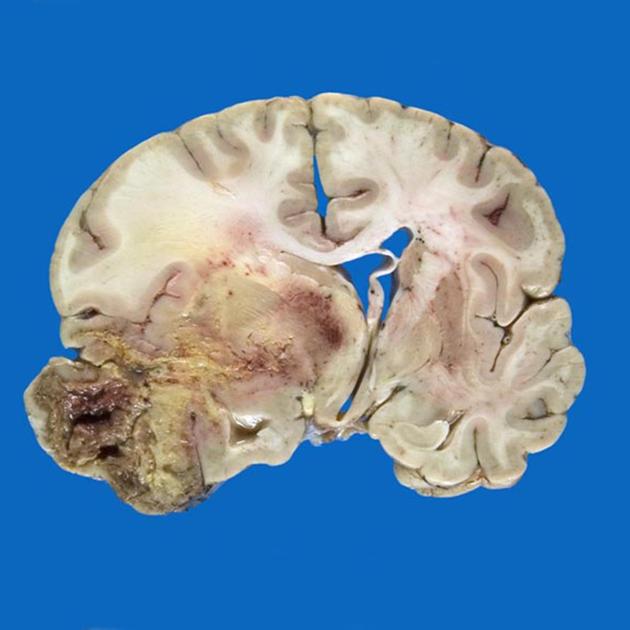
Glioblastoma (9x8x7cm). The image is taken from radiopaedia.org.
Causes and Risk Factors
The exact causes of glioblastoma are not fully understood, but several risk factors have been identified:
- Ionizing radiation exposure: Previous exposure to high doses of ionizing radiation, particularly to the head and neck region, is a well-established risk factor for glioblastoma.
- Genetic predisposition: Certain genetic conditions, such as neurofibromatosis type 1 (NF1), Li-Fraumeni syndrome, and Turcot syndrome, are associated with an increased risk of developing glioblastoma.
- Environmental factors: While the evidence is not conclusive, some studies have suggested potential links between glioblastoma and exposure to certain chemicals, such as pesticides, solvents, and electromagnetic fields.
- Age and gender: As mentioned earlier, the risk of glioblastoma increases with age, and it is slightly more common in men than in women.
It is important to note that most cases of this tumor occur sporadically, without any identifiable risk factors.
Symptoms
The symptoms of glioblastoma can vary depending on the location and size of the tumor within the brain. Common symptoms include:
- Headaches: Persistent and worsening headaches, often accompanied by nausea and vomiting, are common early signs of glioblastoma.
- Seizures: Seizures, either focal (affecting a specific part of the body) or generalized, can occur in some patients with glioblastoma.
- Cognitive and personality changes: Glioblastoma can cause changes in cognitive function, such as memory loss, confusion, and difficulty with speech or comprehension. Personality changes, such as irritability or mood swings, may also occur.
- Neurological deficits: Depending on the location of the tumor, patients may experience neurological deficits, such as weakness, numbness, or loss of coordination in specific parts of the body.
- Visual disturbances: Tumors located near the optic nerves or visual cortex can cause visual problems, such as double vision, blurred vision, or loss of peripheral vision.
Diagnosis
The diagnosis of glioblastoma typically involves a combination of imaging techniques and tissue analysis:
- Imaging studies: Magnetic resonance imaging (MRI) is the primary imaging modality used to detect and characterize brain tumors. MRI scans can provide detailed information about the location, size, and extent of the tumor, as well as its relationship to surrounding brain structures.
- Tissue biopsy or surgical resection: A definitive diagnosis of glioblastoma requires a tissue sample, which can be obtained through a biopsy or surgical resection. The tissue sample is then analyzed by a pathologist to confirm the diagnosis and determine the molecular characteristics of the tumor.
- Molecular testing: Molecular testing, such as genetic and epigenetic analyses, is increasingly being used to identify specific genetic alterations and biomarkers that can help guide treatment decisions and provide prognostic information.
In some cases, additional tests, such as functional MRI (fMRI), positron emission tomography (PET), or magnetic resonance spectroscopy (MRS), may be performed to gather more information about the tumor and its impact on brain function.
Glioblastoma Treatment Options
The treatment of glioblastoma typically involves a multidisciplinary approach, combining various modalities to maximize the chances of successful treatment and improve patient outcomes. The standard treatment regimen includes:
- Surgical resection: Whenever possible, surgical removal of as much of the tumor as safely possible is the first line of treatment. This procedure, known as maximal safe resection, aims to reduce the tumor burden and alleviate symptoms caused by increased intracranial pressure.
- Radiation therapy: After surgery, patients typically undergo radiation therapy, which involves the use of high-energy radiation beams to target and destroy any remaining cancer cells. Various techniques, such as intensity-modulated radiation therapy (IMRT) and stereotactic radiosurgery, may be employed to deliver precise and targeted radiation doses while minimizing damage to surrounding healthy brain tissue.
- Chemotherapy: Concurrent with radiation therapy, patients often receive chemotherapy. Chemotherapy helps to enhance the effectiveness of radiation therapy and target any remaining cancer cells that may have spread beyond the primary tumor site.
In addition to these standard treatments, several emerging and investigational therapies are being explored for the treatment of this tumor:
- Targeted therapies: These therapies target specific molecular pathways or genetic alterations that drive tumor growth and progression. Examples include anti-angiogenic agents and various tyrosine kinase inhibitors.
- Immunotherapy: Immunotherapies aim to harness the body’s immune system to recognize and attack cancer cells. Approaches such as immune checkpoint inhibitors, cancer vaccines, and adoptive cell therapies (e.g., CAR T-cell therapy) are being investigated for glioblastoma.
- Tumor treating fields (TTFields): This non-invasive treatment involves the use of alternating electric fields to disrupt the division and proliferation of cancer cells. TTFields are approved for use in combination with chemotherapy for the treatment of newly diagnosed and recurrent glioblastoma.
More information about completed and ongoing clinical trials can be found here – clinicaltrials.gov.
Patient Survivorship
Glioblastoma is a challenging and life-threatening condition, and survivorship is a significant concern for patients and their families. While the overall prognosis remains poor, there is a small percentage of patients who achieve long-term survival, defined as living for five years or more after diagnosis. Factors that may contribute to improved survival include:
- Younger age at diagnosis: Younger patients generally have better outcomes compared to older patients.
- Favorable molecular characteristics: Certain molecular features can influence treatment response and survival.
- Extent of surgical resection: Patients who undergo complete or near-complete surgical resection tend to have better outcomes compared to those with residual tumor burden.
- Access to clinical trials and novel therapies: Participation in clinical trials and access to emerging treatments may improve survival outcomes for some patients.
Problems During and After Treatment and How to Manage Them
Patients with glioblastoma may experience various challenges and side effects during and after treatment, which can significantly impact their quality of life. Some common problems and strategies for managing them include:
- Fatigue: Fatigue is a common side effect of radiation therapy, chemotherapy, and the tumor itself. Strategies to manage fatigue include getting adequate rest, maintaining a balanced diet, and engaging in light exercise as tolerated.
- Cognitive and neurological deficits: Glioblastoma and its treatments can cause cognitive impairments, such as memory loss, difficulty with concentration, and language deficits. Neurological deficits, such as weakness, numbness, or loss of coordination, may also occur. Rehabilitation services, including physical therapy, occupational therapy, and speech therapy, can help manage these deficits.
- Seizures: Patients with glioblastoma may experience seizures, which can be managed with anti-seizure medications (anticonvulsants).
- Psychological and emotional distress: The diagnosis and treatment of glioblastoma can be emotionally and psychologically challenging for patients and their families. Counseling, support groups, and mental health services can provide valuable support and coping strategies.
- Nutritional challenges: Glioblastoma and its treatments can affect appetite and nutritional status. Consultation with a dietitian or nutritionist can help ensure adequate nutritional intake and address any specific dietary needs or concerns.
- Palliative care: As glioblastoma progresses, palliative care services can provide comprehensive support to manage symptoms, alleviate suffering, and improve overall quality of life for patients and their families.
In a video produced by the National Cancer Institute, Barbara shares her experience caring for her husband.
Conclusion
Glioblastoma is a formidable and challenging condition that requires a multidisciplinary approach to treatment and supportive care. While the prognosis remains poor, ongoing research and clinical trials offer hope for improved outcomes and novel therapeutic strategies. Patients and their families should stay informed about the latest developments and work closely with their healthcare team to make informed decisions about their treatment and care.
By understanding the prevalence, types, causes, symptoms, diagnosis, and treatment options for glioblastoma, as well as the potential problems and strategies for managing them, patients can better navigate this complex and challenging journey. With the support of healthcare professionals, loved ones, and patient advocacy organizations, individuals affected by glioblastoma can strive to maintain the best possible quality of life and access the resources and support they need.
Watch Ryan’s journey as a glioblastoma patient in a video produced by the Ivy Brain Tumor Center.
Sources
- American Cancer Society – cancer.org
- National Cancer Institute – cancer.gov
- American Brain Foundation
- American Society of Clinical Oncology – asco.org
- Glioblastoma Foundation
- Brain Tumour Research
- Canadian Cancer Society – cancer.ca
- Glioblastoma: An Update in Pathology, Molecular Mechanisms and Biomarkers – International Journal of Molecular Sciences
