Liver Cancer: What patients should know about
Introduction
Liver cancer is a serious condition that occurs when abnormal cells in the liver grow uncontrollably. It can be classified into primary liver cancer, which starts in the liver, and secondary liver cancer, which spreads to the liver from other parts of the body. Understanding the causes, risk factors, types, symptoms, diagnosis, prognosis, treatment options, and ongoing research is crucial for patients and their families.
Liver Cancer Causes and Risk Factors
Causes
The exact cause of liver cancer is not always clear, but it often involves changes in the DNA of liver cells. These changes can lead to uncontrolled cell growth and the formation of tumors.
Risk Factors
Several factors can increase the risk of developing liver cancer:
- Cirrhosis: This condition involves scarring of the liver due to long-term damage. It can be caused by chronic alcohol abuse, hepatitis B or C infections, and other liver diseases. Cirrhosis develops when liver cells are damaged and replaced by scar tissue. Most cirrhosis in the United States is caused by regularly drinking too much alcohol, called alcohol abuse.
Other causes of liver cirrhosis are non-alcoholic fatty liver disease (NAFLD), viral hepatitis (types B and C), too much iron in the liver from a disease called hemochromatosis, and some other rare types of chronic liver disease. The combination of alcohol abuse and hepatitis virus infection puts people at high risk of cirrhosis and hepatocellular carcinoma (HCC), which is a type of liver cancer. - Obesity, NAFLD, and diabetes: Obesity causes fat to be deposited in the liver, which leads to NAFLD. Over the past decade, strong evidence has emerged suggesting that NAFLD and diabetes, a related disease, are increasingly important risk factors for HCC in the United States.
- Viral hepatitis: Hepatitis viruses are viruses that infect the liver. The two common types are hepatitis B and hepatitis C. Viral hepatitis is the largest risk factor for liver cancer worldwide. Hepatitis C has become much more common than hepatitis B because there is no vaccine to prevent hepatitis C. Viral hepatitis can be passed from person to person through exposure to blood or bodily fluids. This can happen through physical injury or trauma, by sharing needles during drug use or the tattooing process, or by sexual contact.
In the case of hepatitis B, an unborn baby or infant can get the virus if the mother has it. This can be avoided by vaccinating the baby. If the patient develops acute hepatitis B or C and then “clear the virus,” he may recover completely from the acute infection. Only people who do not clear the virus and have a persistent infection have an increased risk. - Age: In the United States, adult primary liver cancer occurs most often in people older than 60.
- Sex: Men are more likely than women to develop liver cancer.
- Environmental factors: Some environmental factors may increase the risk of liver cancer, such as exposure to certain chemicals or eating food contaminated with aflatoxin. Aflatoxin is a toxin made by a mold that can grow on stored nuts and grains. There is less risk of this in the United States.
Risk factors are cumulative. This means that having more than one risk factor increases a person’s risk of developing liver cancer more. For instance, a person who carries both hepatitis B and C has a higher risk than a person carrying one type of the virus. Similarly, a person with hepatitis C who also drinks alcohol has a higher risk.
Liver Cancer Types
Hepatocellular Carcinoma (HCC)
HCC is the most common type of primary liver cancer. It starts in the main liver cells called hepatocytes. It is often associated with chronic liver diseases like hepatitis and cirrhosis.
Fibrolamellar Carcinoma
This rare subtype of HCC typically affects younger individuals and is not usually linked with cirrhosis or hepatitis infections.
Cholangiocarcinoma (Bile Duct Cancer)
This cancer starts in the bile ducts, which are tubes that carry bile from the liver to the gallbladder and small intestine. It can be intrahepatic (inside the liver) or extrahepatic (outside the liver).
Angiosarcoma
This rare and aggressive cancer starts in the blood vessels of the liver. It is often diagnosed at an advanced stage.
Hepatoblastoma
This rare type of liver cancer primarily affects young children, usually under the age of 3.
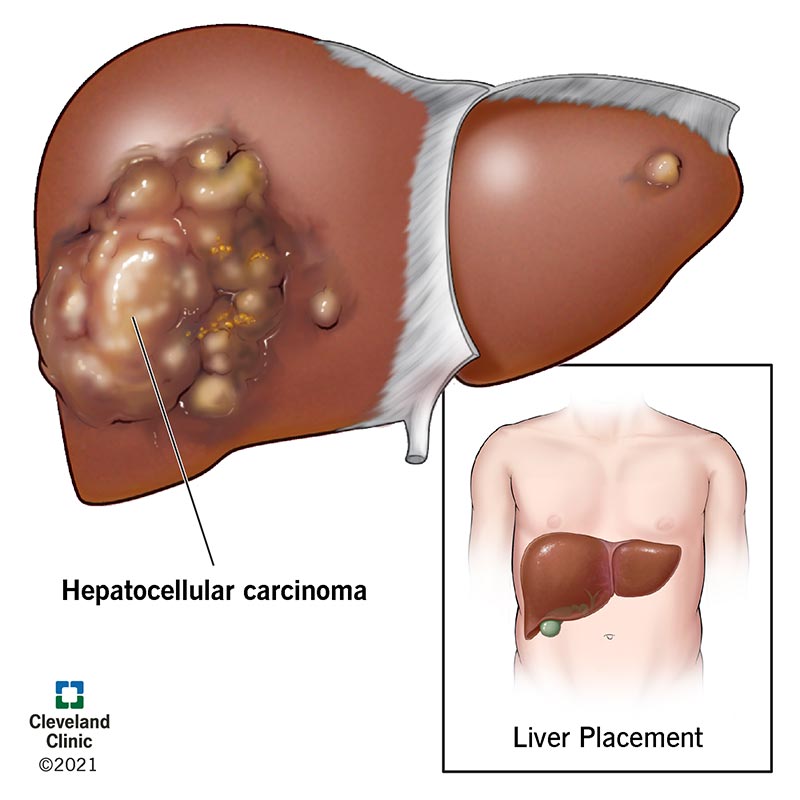
This image is taken from – clevelandclinic.org
Liver Cancer Symptoms
Liver cancer symptoms often do not appear until the disease is advanced. When symptoms do occur, they may include:
- Weight loss: Unintentional weight loss is a common symptom.
- Loss of appetite: Patients may feel full after eating small amounts of food.
- Nausea and vomiting: These symptoms can be persistent.
- Abdominal pain: Pain may be felt in the upper right side of the abdomen or near the right shoulder blade.
- Swelling: The abdomen may swell due to fluid buildup (ascites).
- Jaundice: Yellowing of the skin and eyes can occur due to liver dysfunction.
- Itching: This can be caused by bile salts accumulating in the skin.
- Fatigue: Patients may feel unusually tired or weak.
- Fever: Some patients may experience a fever.
Diagnosis
Diagnosing liver cancer involves several tests and procedures to accurately identify the presence and extent of the disease. These tests help determine the best course of treatment and monitor the progression of the cancer.
Physical Examination
A thorough physical examination may be performed to check for any abnormalities in the liver, spleen, and abdomen. This includes feeling for lumps, swelling, or changes in the size and shape of these organs. Signs of jaundice, which is a yellowing of the skin and eyes that can indicate liver dysfunction, may also be looked for. Additionally, the presence of ascites, an abnormal accumulation of fluid in the abdomen, may be checked as it is often associated with advanced liver disease.
Blood Tests
Blood tests are essential in diagnosing liver cancer. These tests can reveal abnormalities in liver function and measure levels of alpha-fetoprotein (AFP), a protein that can be elevated in liver cancer. Elevated AFP levels can indicate the presence of hepatocellular carcinoma (HCC), the most common type of primary liver cancer. However, elevated AFP levels can also be seen in other conditions such as hepatitis and cirrhosis, so additional tests are often required to confirm a diagnosis.
Imaging Tests
Imaging tests provide detailed pictures of the liver and help identify tumors and other abnormalities. Common imaging tests used in diagnosing liver cancer include:
- Ultrasound: This test uses sound waves to create images of the liver. It is often the first imaging test performed and can detect tumors and other abnormalities in the liver.
- CT Scan: A CT scan provides detailed cross-sectional images of the liver and can help identify tumors, their size, and their location. It is particularly useful in assessing the extent of the cancer and whether it has spread to other parts of the body.
- MRI: MRI uses magnetic fields to create detailed images of the liver. It is especially helpful in determining the extent of the cancer and in distinguishing between benign and malignant tumors.
- PET Scan: This test uses a small amount of radioactive glucose to detect cancer cells in the body. Cancer cells absorb glucose more rapidly than normal cells, making them visible on the scan. PET scans are useful in detecting the spread of cancer to other parts of the body.
Biopsy
A biopsy involves removing a small sample of liver tissue to be examined under a microscope. This procedure can confirm the presence of cancer cells and provide information about the type and stage of the cancer. There are different methods of performing a liver biopsy, including:
- Percutaneous Biopsy: A needle is inserted through the skin and into the liver to obtain a tissue sample. This is the most common method and is usually guided by ultrasound or CT imaging.
- Transjugular Biopsy: A needle is inserted into a vein in the neck and threaded through the veins to the liver to obtain a tissue sample. This method is used for patients with bleeding disorders or ascites.
- Laparoscopic Biopsy: A laparoscope (a thin, lighted tube with a camera) is inserted through a small incision in the abdomen to obtain a tissue sample. This method allows for visual inspection of the liver and other organs.
These diagnostic tests and procedures are crucial in accurately diagnosing liver cancer and determining the most effective treatment plan. Early detection and diagnosis can significantly improve the chances of successful treatment and better outcomes for patients.
Liver Cancer Prognosis
The prognosis for liver cancer depends on several factors, including the stage of the cancer, the patient’s overall health, and the underlying cause of the liver disease. Early-stage liver cancer that can be surgically removed has a better prognosis than advanced-stage cancer. However, liver cancer is often diagnosed at a later stage, making treatment more challenging.
Treatment and Side Effects for Different Liver Cancers
Hepatocellular Carcinoma (HCC)
Surgery
- Partial Hepatectomy: Removing part of the liver where the tumor is located. This is an option for early-stage HCC.
- Liver Transplant: Replacing the entire liver with a healthy donor liver. This may be considered if the cancer has not spread outside the liver.
Ablation Therapy
- Radiofrequency Ablation (RFA): Using heat to destroy cancer cells.
- Cryoablation: Freezing cancer cells to kill them.
- Ethanol Injection: Injecting alcohol directly into the tumor.
Embolization
- Transarterial Chemoembolization (TACE): Delivering chemotherapy directly to the tumor and blocking its blood supply.
- Radioembolization: Using radioactive beads to block blood supply and deliver radiation to the tumor.
Other Treatments
- Radiation Therapy: Using high-energy rays to kill cancer cells and shrink tumors.
- Targeted Therapy: Drugs like sorafenib and lenvatinib that target specific molecules involved in cancer growth.
- Immunotherapy: Drugs like nivolumab and pembrolizumab that help the immune system recognize and attack cancer cells.
- Chemotherapy: Using drugs to kill cancer cells, often combined with other treatments.
Liver Angiosarcoma
- Surgery: Complete surgical removal of the tumor and surrounding healthy tissue is the primary curative treatment for localized angiosarcoma.
- Chemotherapy: May be used in combination with surgery or for palliative care.
- Radiation Therapy: Generally not effective for liver angiosarcoma.
- Embolization: Techniques like transarterial chemoembolization (TACE) may be used to control bleeding or deliver chemotherapy directly to the tumor.
Hepatoblastoma (Childhood Liver Cancer)
- Surgery: Partial hepatectomy (removing part of the liver) or liver transplant are common treatments for resectable hepatoblastoma.
- Chemotherapy: Often used before surgery to shrink the tumor or after surgery to eliminate any remaining cancer cells.
- Radiation Therapy: May be used in some cases of unresectable or high-risk hepatoblastoma.
Regardless of the liver cancer type, patients should discuss potential side effects like fatigue, nausea, vomiting, loss of appetite, and hair loss with their healthcare team.
Newest Options and Ongoing Trials
Research is ongoing to find new and more effective treatments for liver cancer. Clinical trials are testing new drugs, combinations of treatments, and innovative therapies. Patients may consider participating in clinical trials to access cutting-edge treatments and contribute to medical research.
More information about ongoing clinical trials can be found on clinicaltrials.gov
Patient Survivorship
Survivorship care is an important aspect of liver cancer treatment. It involves regular follow-up visits to monitor for cancer recurrence, manage side effects, and address any physical or emotional challenges. Support groups and counseling can help patients and their families cope with the impact of liver cancer.
Follow-Up Care
After completing treatment, liver cancer survivors need to have regular follow-up appointments with their healthcare team. These visits are crucial for monitoring the patient’s health, checking for signs of cancer recurrence, and managing any long-term side effects of treatment. Typically, follow-up care includes physical examinations, blood tests, and imaging tests such as ultrasounds, CT scans, or MRIs. The frequency of these visits may vary depending on the individual’s condition and the type of treatment they received. For instance, patients who have undergone surgery, liver transplants, or ablation/embolization procedures may have follow-up visits every three to six months for the first two years, and then every six to twelve months thereafter.
Managing Long-Term Side Effects
Liver cancer treatment can result in long-lasting side effects that may not appear until months or even years after treatment has ended. Common long-term side effects include fatigue, pain, digestive issues, and changes in appetite. It is important for survivors to communicate any new or persistent symptoms to their healthcare team so that appropriate management strategies can be implemented. For example, fatigue can be managed through regular physical activity, balanced nutrition, and adequate rest.
Emotional and Psychological Support
The emotional and psychological impact of liver cancer can be significant. Survivors may experience feelings of anxiety, depression, or fear of cancer recurrence. Support groups and counseling can provide a safe space for survivors to share their experiences and receive emotional support. Oncology social workers and mental health professionals can help survivors develop coping strategies and address any psychological challenges they may face.
Lifestyle Changes
Adopting a healthy lifestyle is an important part of survivorship care. Liver cancer survivors are encouraged to follow established guidelines for good health, such as not smoking, limiting or avoiding alcohol, eating a balanced diet, exercising regularly, and managing stress. Regular physical activity can help rebuild strength and energy levels, while a healthy diet can support overall well-being. Survivors should work closely with their healthcare team to develop a personalized plan that meets their specific needs.
Support Resources
There are numerous resources available to support liver cancer survivors and their families. Organizations such as the American Cancer Society, CancerCare, and the American Liver Foundation offer educational materials, support groups, financial assistance, and counseling services. These resources can help survivors navigate the challenges of life after cancer and connect with others who have had similar experiences.
Building a Support Network
Having a strong support network is essential for liver cancer survivors. Family, friends, and caregivers can provide emotional support, practical assistance, and encouragement. Support groups, both in-person and online, offer opportunities for survivors to connect with others who understand their experiences. Building a support network can help survivors feel less isolated and more empowered in their journey.
Returning to Work
Returning to work after liver cancer treatment can be challenging. Survivors may need to make adjustments to their work schedule or responsibilities to accommodate their health needs. It is important for survivors to communicate with their employers about their situation and explore options such as flexible work hours or telecommuting. Support from colleagues and supervisors can also make the transition back to work smoother.
This informative video is taken from Roche
Conclusion
Liver cancer is a complex disease with various causes, risk factors, and treatment options. Early detection and treatment are crucial for improving outcomes. Patients should work closely with their healthcare team to understand their diagnosis, explore treatment options, and manage their care. Ongoing research and clinical trials offer hope for new and more effective treatments in the future.
Resources
- Liver Cancer: Risk Factors and Prevention – cancer.net
- Signs and Symptoms of Liver Cancer – cancer.org
- Liver Cancer Diagnosis – cancer.gov
- Risks and Causes for Liver Cancer – cancerresearchuk.org
- Risk Factors and Prevention of Liver Cancer: A Bibliometric and Visual Analysis – PubMed
- Clinical Practice Guidelines For the Management of Hepatocellular Carcinoma: A Systematic Review
- The 100 most influential manuscripts on hepatocellular carcinoma – PubMed
- Immunotherapies for hepatocellular carcinoma – Nature.com
- Hepatocellular carcinoma | Radiology Reference Article – Radiopedia.org
- Hepatocellular carcinoma | Nature Reviews Disease Primers – Nature.com
- Hepatocellular carcinoma. An overview | Annals of Hepatology