Hypopharyngeal Cancer: What patients should know about
Hypopharyngeal Cancer
Hypopharyngeal cancer is a type of cancer that affects the lower part of the throat, known as the hypopharynx. Despite its relatively rare occurrence, it can present significant challenges due to its location and subtle symptoms.
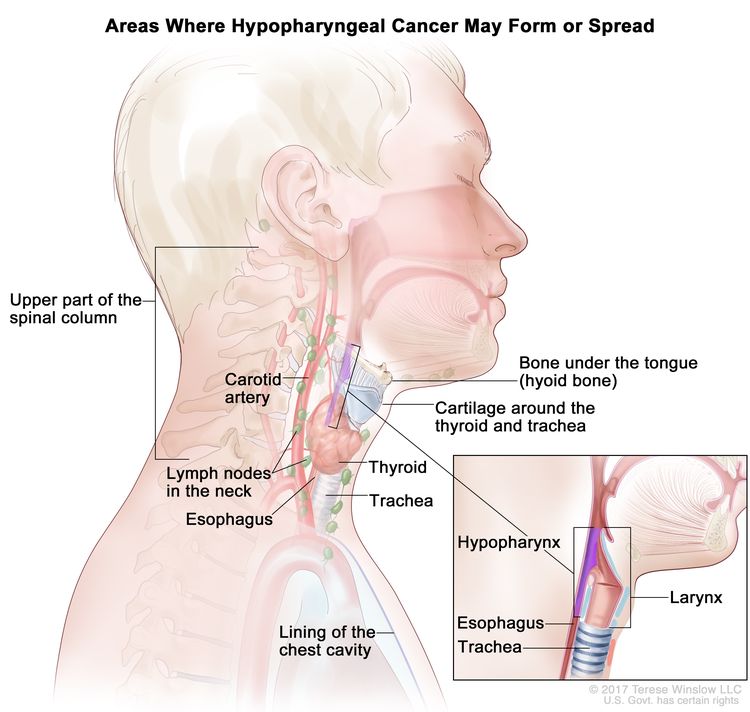
This image is taken from cancer.gov.
Prevalence
Hypopharyngeal cancer accounts for approximately 7% of all cancers of the upper aerodigestive tract and less than 3,000 new cases are diagnosed annually in the United States. It is more common in men than women, with a male-to-female ratio of about 4:1, and typically affects individuals over 50. Hypopharyngeal cancer is exceedingly rare in children.
Causes and Risk Factors
Hypopharyngeal cancer is primarily caused by tobacco use and excessive alcohol consumption. The major risk factors include:
- Tobacco Use: Smoking cigarettes, cigars, pipes, or chewing tobacco/snuff significantly increases the risk of developing hypopharyngeal cancer. The more tobacco is used and the longer the duration of use, the greater the risk.
- Alcohol Consumption: Heavy and frequent alcohol intake raises the risk of hypopharyngeal cancer. When combined with tobacco use, the risk is multiplied substantially.
Other risk factors include:
- Occupational Exposures: Prolonged exposure to certain chemicals, wood dust, paint fumes, and asbestos in industries like metalworking, petroleum, construction, and textiles can increase risk.
- Poor Nutrition: Diets lacking in vitamins A and E, and low intake of fresh fruits and vegetables may contribute to higher risk.
- Gender: Men are 4-5 times more likely to develop hypopharyngeal cancer than women, likely due to higher rates of tobacco and alcohol use.
- Age: Risk increases with age, and over half of cases occur in people aged 65 or older.
- Race/Ethnicity: Hypopharyngeal cancer is more common among Caucasians and African Americans compared to Asian and Hispanic populations.
- Genetic Syndromes: Rare inherited conditions like Fanconi anemia, dyskeratosis congenita, and Plummer-Vinson syndrome significantly elevate the risk.
- Human Papillomavirus (HPV) Infection: Infection with certain strains of HPV, transmitted through sexual activity, may increase the risk in some cases.
Avoiding tobacco products, limiting alcohol intake, maintaining a balanced diet, and getting the HPV vaccine can help reduce the risk of developing hypopharyngeal cancer. There are currently no proven screening methods for early detection of hypopharyngeal cancer, so prevention through lifestyle changes is critical.
Types
The most common type of hypopharyngeal cancer is squamous cell carcinoma, accounting for around 95% of cases. Other rare types of hypopharyngeal cancer include:
- Adenocarcinoma
- Sarcoma (e.g. chondrosarcoma, synovial sarcoma arising from connective tissues)
- Non-epidermoid carcinomas
- Minor salivary gland cancers (from minor salivary glands in the hypopharynx)
- Lymphomas
- Neuroendocrine tumors
- Plasmacytomas
However, squamous cell carcinoma originating from the mucosal lining of the hypopharynx is by far the predominant histological type seen in hypopharyngeal cancer patients. The other types mentioned above are extremely rare in this anatomic site.
Staging
- Stage I: Cancer is limited to one area of the hypopharynx or has a tumor ≤2 cm.
- Stage II: Tumor is >2 cm but ≤4 cm without larynx involvement, or found in multiple hypopharyngeal areas or nearby tissues.
- Stage III: Tumor is >4 cm, or spread to larynx/esophagus, possibly affecting small lymph node (<3 cm) on the same side of the neck.
- Stage IVA: Spread to nearby structures like cartilage, thyroid, or soft tissue; possibly affecting lymph node (3-6 cm) or multiple smaller nodes.
Stage IVB: Spread to upper spinal muscles, carotid artery, or chest cavity lining, or larger lymph nodes; any tumor size.
Stage IVC: Spread beyond hypopharynx to distant body parts; any tumor size.
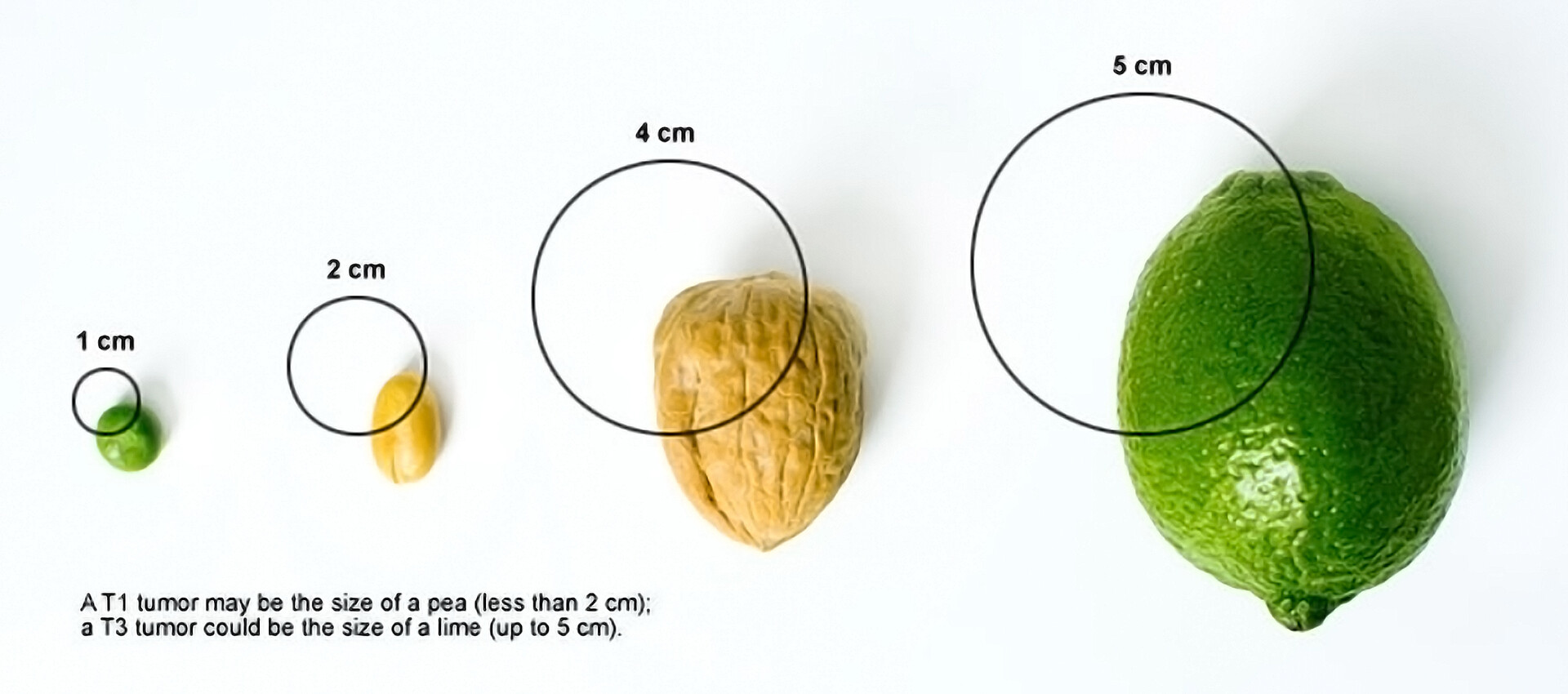
Tumor sizes. This image is taken from storymd.com.
Symptoms
The key symptoms of hypopharyngeal cancer include:
- Difficulty swallowing (dysphagia) or a feeling that something is stuck in the throat
- Persistent sore throat or pain when swallowing
- Ear pain (otalgia) or discomfort, often referred from the throat via the Arnold nerve
- Hoarseness or changes in voice quality
- Breathing difficulties or noisy breathing (stridor)
- Coughing up blood (hemoptysis)
- Painless lump or mass in the neck, often indicating lymph node involvement
- Weight loss
Later symptoms as the cancer advances can include:
- Vocal cord paralysis causing hoarseness
- Invasion of surrounding structures like the larynx or esophagus
- It’s important to note that early-stage hypopharyngeal cancers may not cause any noticeable symptoms initially.
Symptoms often appear later when the tumor has grown larger or spread, leading to a delay in diagnosis. Persistent symptoms like difficulty swallowing, sore throat, ear pain, or a neck mass should prompt further evaluation by a doctor to rule out hypopharyngeal cancer, especially in individuals with risk factors like smoking and alcohol use.
Diagnosis
The primary techniques utilized for detecting hypopharyngeal cancer involve:
- Physical Examination: Inspection of the nose, mouth, throat, and neck region. Palpation of the neck to check for swollen lymph nodes.
- Endoscopy: Flexible fiberoptic endoscopy to visualize the hypopharynx. Performed in the office with local anesthesia/numbing.
- Biopsy: Taking a tissue sample from any suspicious growths. Can be done during endoscopy or under general anesthesia in the operating room. The biopsy is examined by a pathologist to confirm the cancer diagnosis.
- Imaging Tests:
- CT Scan – Provides detailed images to assess tumor extent and spread
- MRI Scan – Useful for evaluating soft tissue involvement
- PET Scan – Helps detect if cancer has spread to lymph nodes or other areas
- Fine Needle Aspiration: Using a small needle to extract cells from swollen lymph nodes. Cells are examined for the presence of cancer.
After the initial diagnosis, accurate staging is crucial to guide treatment planning. This involves combining the results from the physical exam, endoscopy, imaging tests, and biopsy to determine the extent of the tumor (T), lymph node involvement (N), and any distant metastasis (M). A multidisciplinary team involving head and neck surgeons, radiation and medical oncologists, pathologists, and other specialists comprehensively evaluates all test results to establish the hypopharyngeal cancer diagnosis and staging.
Treatment
The main treatment approaches for hypopharyngeal cancer include:
- Surgery: Primary surgical treatment involves the removal of the tumor and affected lymph nodes in the neck (neck dissection). Specific surgical procedures include:
-
- Partial pharyngectomy (removal of part of the hypopharynx)
- Total pharyngectomy (removal of the entire hypopharynx)
- Laryngopharyngectomy (removal of the larynx and part of the hypopharynx)
Reconstructive surgery may be needed after major resections to restore swallowing and speech functions. Surgery may be followed by radiation therapy or chemoradiation.
- Radiation Therapy: External beam radiation therapy is a standard treatment, either alone or combined with chemotherapy. Intensity-modulated radiation therapy (IMRT) is commonly used to precisely target the tumor. Radiation may be given before surgery (neoadjuvant) or after surgery (adjuvant).
- Chemotherapy: Chemotherapy drugs like cisplatin, carboplatin, and 5-FU are often given concurrently with radiation therapy (chemoradiation). Induction or neoadjuvant chemotherapy may be given before surgery or radiation. Chemotherapy can also be used for palliative treatment in advanced cases.
- Targeted Therapy and Immunotherapy: Targeted therapies like cetuximab (EGFR inhibitor) may be combined with radiation. Immunotherapy drugs like pembrolizumab and nivolumab (PD-1 inhibitors) are newer options, especially for recurrent disease.
The treatment approach depends on the stage of the cancer, the patient’s overall health, and the goals of care (curative vs palliative). A multidisciplinary team involving surgeons, radiation, and medical oncologists plans the optimal multimodal treatment for each patient.
Prognosis
Hypopharyngeal cancer generally has a poor prognosis compared to other head and neck cancers, primarily due to its late presentation and early spread to lymph nodes. The median overall survival is around 1 year after diagnosis. Key prognostic factors that influence survival include:
- Stage at Diagnosis: The stage is the most important prognostic factor. Earlier-stage tumors have a significantly better prognosis than advanced-stage cancers. Unfortunately, most hypopharyngeal cancers are diagnosed at an advanced stage (stage III or IV) when the tumor has invaded surrounding tissues and lymph nodes.
- Lymph Node Involvement: The number of lymph nodes containing cancer cells at diagnosis is a crucial prognostic indicator. More extensive lymph node metastasis is associated with poorer outcomes.
- Depth of Invasion: Tumors that have deeply invaded surrounding structures like muscles, nerves, bone, cartilage and blood vessels have a worse prognosis compared to more superficial lesions.
- Nutritional Status: Poor nutrition, often linked to heavy tobacco/alcohol use, can negatively impact a patient’s ability to tolerate treatment and worsen outcomes.
- Performance Status: Patients with a higher performance status, reflecting their ability to carry out daily activities, tend to better tolerate treatments and have improved survival.
Other prognostic factors include:
- Age (worse prognosis in older patients)
- Sex (women tend to present at earlier stages)
- Comorbidities (presence of other health issues like heart/lung disease)
- Tumor subsite (pyriform sinus/aryepiglottic fold tumors have better outcomes)
Overall, the 5-year survival rate for all stages of hypopharyngeal cancer is approximately 25-30%. However, survival varies greatly based on the stage at presentation and the above prognostic factors. Early detection is crucial, as advanced-stage hypopharyngeal cancers have extremely poor outcomes despite aggressive multimodality treatment approaches.
Recurrence
This cancer has a high risk of recurrence after initial treatment, with early recurrence within 6 months being quite common. The treatment approach for recurrent hypopharyngeal cancer depends on factors such as the location and size of the recurrent tumor, previous treatments received, and the patient’s overall health.
Options for managing recurrent disease include surgery (if resectable), re-irradiation, chemotherapy, chemoradiation, targeted therapy (e.g., cetuximab), and immunotherapy. However, radiation therapy alone for unresectable cases has a high local recurrence rate of about 70%, highlighting the need for multimodal treatment approaches.
Additionally, patients who have had hypopharyngeal cancer are at an increased risk of developing a second primary cancer in the head and neck region, emphasizing the importance of frequent and careful follow-up. Close monitoring and appropriate selection of multimodal treatment based on recurrence patterns and patient factors are crucial for managing recurrent hypopharyngeal cancer effectively.
Patient’s Survivorship
Patients with hypopharyngeal cancer face numerous challenges during and after treatment that can significantly impact their quality of life and survivorship.
Physical Challenges
- Dysphagia (Swallowing Difficulties)
A common side effect of surgery, radiation, and chemoradiation therapy
Can lead to malnutrition, dehydration, aspiration pneumonia
Management: Swallowing therapy, dietary modifications, temporary feeding tubes - Dysphonia (Voice Changes)
Partial or total loss of voice due to treatment effects on the larynx
Can impair communication and social interactions
Management: Voice therapy, electrolaryngeal devices, surgical voice restoration - Fatigue
Persistent fatigue is common during and after treatment
This can be exacerbated by poor nutrition, pain, and emotional distress
Management: Exercise, energy conservation techniques, treatment of underlying causes - Chronic Pain
Pain can result from surgery, radiation-induced fibrosis, or neuropathy
This can be localized or diffuse, impacting daily activities
Management: Analgesics, physical therapy, interventional pain management
Psychosocial Challenges
- Body Image and Self-Esteem
Visible disfigurement, scars, and use of prosthetic devices can affect self-image
This may lead to social withdrawal, depression, and intimacy issues
Management: Counseling, support groups, cosmetic interventions - Fear of Recurrence
Anxiety and fear of cancer recurrence are common among survivors
This can lead to hypervigilance and avoidance of follow-up care
Management: Psychoeducation, cognitive-behavioral therapy, support groups - Intimacy and Sexual Function
Treatment effects can impact sexual function and intimacy
This may lead to relationship strain and decreased quality of life
Management: Counseling, medications, intimacy aids, couple’s therapy - Return to Work and Financial Toxicity
Prolonged treatment and recovery can disrupt employment and income
Financial strain can exacerbate stress and impact access to care
Management: Vocational rehabilitation, disability benefits, financial counseling
Multidisciplinary Approach
Addressing these challenges requires a comprehensive, multidisciplinary approach involving:
- Head and neck surgeons, radiation and medical oncologists
- Speech and swallowing therapists, dietitians, physical therapists
- Psychologists, social workers, counselors, and support groups
- Primary care providers for coordinated long-term follow-up
Regular screening, early intervention, and patient education are crucial for optimal survivorship care. Ongoing research aims to develop targeted interventions and supportive care programs to improve the quality of life for hypopharyngeal cancer survivors.
Palliative care
- Importance of Palliative Care: 70-80% of hypopharyngeal cancer patients will require palliative and/or end-of-life care due to the advanced stage at diagnosis and poor prognosis of this disease. Palliative care should be initiated early, at the time of initial diagnosis and treatment planning, to address symptom management and supportive care needs. It helps control common distressing symptoms like pain, difficulty swallowing, breathing issues, nutritional problems, and psychosocial distress. For recurrent or metastatic diseases, palliative chemotherapy, radiation, or immunotherapy may help control tumor growth and relieve symptoms.
- Efficiency and Benefits: Palliative care improves quality of life, patient satisfaction, caregiver burden, and potentially survival in patients with serious illnesses like advanced cancer. It alleviates pain, depression, psychosocial distress, fatigue, and dyspnea while providing information and care planning. Early integration of palliative care results in higher hospice utilization, reduction in aggressive end-of-life care, and modestly extended survival in some cases. Patients receiving early palliative care have fewer depressive symptoms and less aggressive end-of-life care compared to standard oncology care alone. Palliative care interventions have been shown to reduce healthcare costs by decreasing the length of hospital stay and intensity of hospital care.
Recommendations for Patients
- Learn about your specific diagnosis, stage, and treatment options. Don’t hesitate to ask your healthcare team questions to better understand your condition.
- Consider getting a second opinion, especially from experts at major cancer centers experienced in treating hypopharyngeal cancers.
- Discuss all potential treatment approaches with your doctors, including the risks and benefits of surgery, radiation, chemotherapy, and newer options like targeted therapy or immunotherapy.
- Make sure you understand the potential side effects of each treatment modality and how they may impact functions like swallowing, speech, and quality of life.
- Inquire about clinical trials exploring new therapies or supportive care strategies that you may be eligible for.
Prepare for the physical and emotional challenges of treatment by arranging for nutritional support, speech therapy, and counseling services as needed. - Build a support network of family, friends, and patient support groups to help you cope during and after treatment.
- Maintain open communication with your healthcare team about any side effects, concerns, or challenges you face throughout your cancer journey.
- Advocate for yourself and ensure your voice is heard when making treatment decisions aligned with your goals and preferences.
- After treatment, attend all follow-up appointments and discuss any persistent issues or late effects with your providers for proper management.
The key is to be an active participant in your care, seek support resources, and maintain open communication with your healthcare team to optimize your outcomes and quality of life.
Conclusion
Facing hypopharyngeal cancer may seem overwhelming, but understanding it can help you navigate your journey. This type of cancer affects the bottom part of the throat, often diagnosed later due to subtle symptoms like difficulty swallowing or throat pain. However, early detection methods like imaging tests are improving outcomes. Treatment usually involves a combination of surgery, radiation therapy, and chemotherapy. While it may be tough, support groups and counseling services are available to help you through this journey. Stay informed, stay strong, and know you’re not alone.
Jack describes the challenges he faced in social situations due to his laryngeal cancer. Fortunately, nowadays, treatments offer much better outcomes.
Resources
- Compass Oncology – compassoncology.com
- American Cancer Society – cancer.org
- Cancer Research UK – cancerresearchuk.org
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Penn Medicine Abramson Cancer Center – pennmedicine.org
- Hypopharyngeal Cancer – PubMed
- National Cancer Institute – cancer.gov
- Johns Hopkins Medicine – hopkinsmedicine.org
- City of Hope – cancercenter.com
- Hypopharyngeal Cancer: United Kingdom National Multidisciplinary Guidelines – PubMed
- Canadian Cancer Society – cancer.ca
- UC San Diego health Clinical Trials – clinicaltrials.ucsd.edu
- Current Therapeutic Strategies for Patients with Hypopharyngeal Carcinoma – PubMed
- University of California San Francisco UCSF Clinical Trials – clinicaltrials.ucsf.edu
- Management of Advanced-stage Hypopharyngeal Carcinoma – PubMed