Talha Badar: Differentiation syndrome with targeted therapies for myeloid malignancies
Talha Badar, Hematologist/Oncologist at Mayo Clinic, shared a post on X/Twitter:
“Weekend review
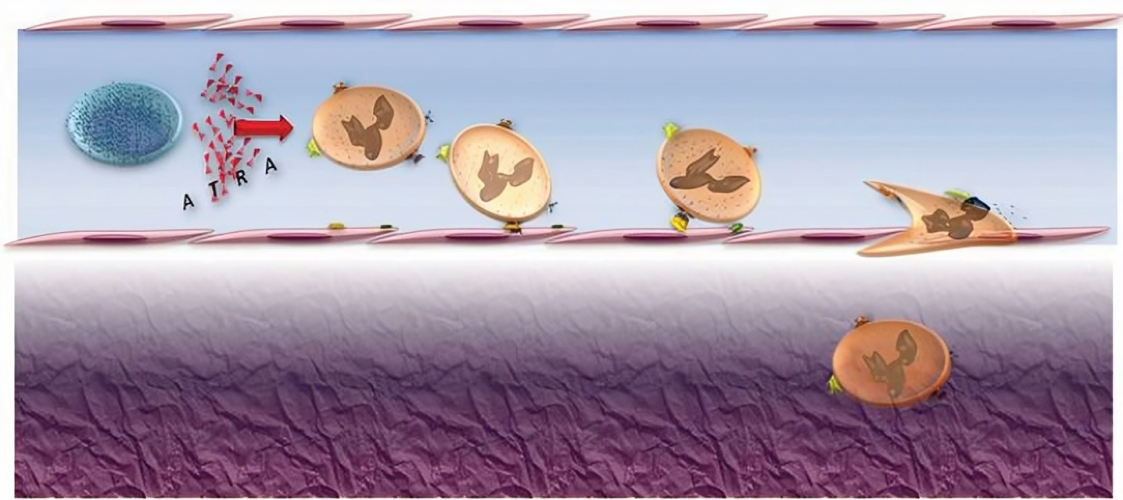
1/6 Differentiation syndrome (DS) with targeted therapies for myeloid malignancies DS characterized by non-infectious related fever, weight gain sec to third spacing (pleural/pericardial effusion) and renal insufficiency. Historically, known to occur with ATRA/ATO, later seen with FLT3i, IDH1/IDH2i, and now with Menin inhibitors. Brief overview on DS beyond APL.
2/6 Differentiation syndrome
Incidence varies with different therapies, ranging from 5%-35%.
Unlike APL, with targeted therapies it occurs later in the treatment (up to 5 months), median days of onset 7-12 days.
Atypical presentation includes pericarditis, myocarditis, ocular manifestation (retinal hemorrhage, macular edema), pancreatitis, sweet syndrome.
Labs/radiological findings ↑ WBC, troponin, pro-BNP. CXR: interstitial edema, pleural effusion, increase cardiothoracic ratio are common findings.
PMID 22220256,12221682, 33307628, 37835461
3/6 Differentiation syndrome with FLT3i
Mechanism: Blocking FLT3 causes dephosphorylation of CEBPA, cause myeloid differentiation ( J Exp Med. 2006; 203(2): 371-381)
Earlier generation of FLT3i, multi-kinase inhibitors such as Sorafenib/Mido, DS is rare.
Gilteritinib, newer generation, selective/potent. DS reported around3%, time onset 2-75 days (N Engl J Med. 2019; 381(18): 1728-1740)
Sign and symptoms are similar. Symptoms resolves with dose interruption/discontinuation.
No correlation between DS and response to therapy. Neutrophil surge is less prominent than seen in APL. Commonly seen with DNMT3A and NPM1 co-mutated (need to be studied further).
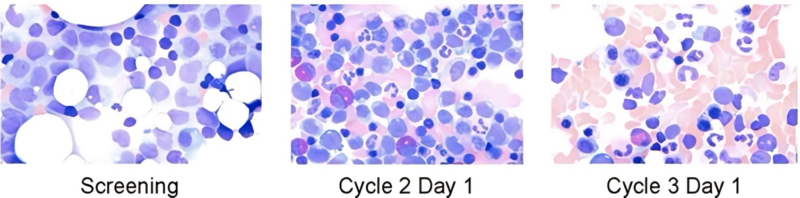
4/6 Differentiation syndrome with IDH1/IDH2i
IDH1i (Tibsovo), DS reported in 11%, G3 5%. (N Engl J Med. 2018; 378(25): 2386-2398)
Median time 29 days (5-59 days)
In trials, managed with hydrea, steroids and diuretics.
Olutasidenib another IDH1i, reported 13%. Successfully managed with dexamethasone, hydroxyurea, and supportive care, as well as temporary interruption.
IDH2i, DS reported in 14% (JAMA Oncol. 2018; 4(8): 1106-1110) Median onset 30 days (7-129 days). No association with DS and response. DS was less common when IDHi were given with chemo, 2.2%
Visit the article website.
5/6 Differentiation syndrome with Menin inhibitors
In pivotal Revumenib study reported around 16%, all G2. Median time of onset 18 days (5-41). Managed with hydrea, steroids. Treatment was not interrupted for the most part.
Ziftomenib, KOMET-001 trial, DS reported in 4/20 pts with NPM1mAML. Mainly G1/2 managed with hydrea and steroids.
Biomea (BMF-219) another menin inhibitor, DS reported in 13%of pts.
6/6 Conclusion: leusm differentiation syndrome
Unlike APL, DS with other targeted therapies have late onset.
Neutrophil surge is less pronounced.
No significant correlation between DS and response to therapy.
Mortality rates are low and rarely requires treatment interruptions.
Ref: really useful article by Dr. Amir Fathi.”
Source: Talha Badar/X